July's Case of the Month- 2022
Sonographer: Meredith Adams, DVM
July 2022 Case of the Month - Left Atrial Rupture in a Chihuahua
Patient Information
Age: 12 years
Gender: Spayed Female
Breed: Chihuahua
Weight: 10.3 pounds
History
Presented for echocardiogram due to heart murmur since July 2021, 5 month history of coughing, and recent finding of ascites. An abdominocentesis was performed 2 days prior to the echocardiogram and the patient had been started on Furosemide 10mg orally every 12 hours.
Echocardiogram procedure
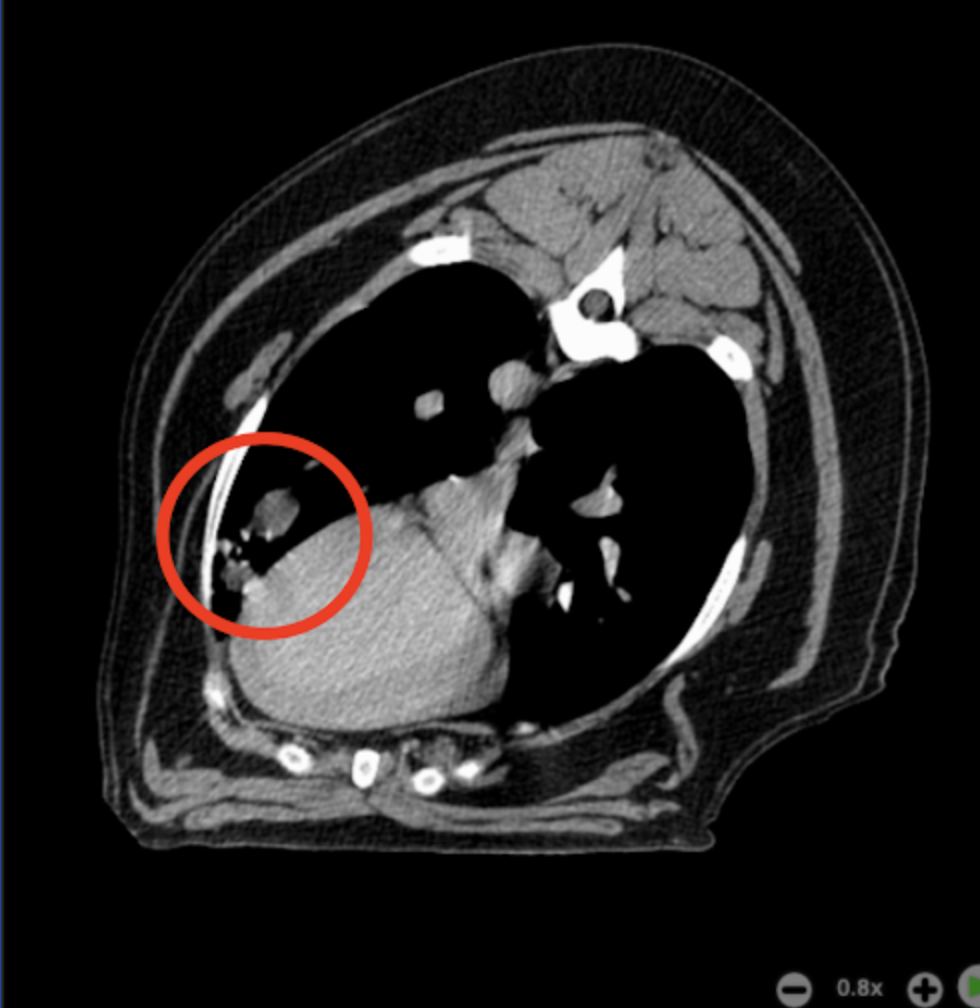
Tipper was bright, alert, and responsive at the beginning of her procedure. A mild amount of pericardial effusion was initially noted at the beginning of the scan. About halfway through the echocardiogram, the volume of pericardial effusion rapidly increased, the patient became acutely lethargic and the heart rate dropped. Mask O2 was delivered and a pericardiocentesis was performed due to the patient’s clinical decline and concern for cardiac tamponade. Only about 4mL of non-clotting blood was obtained from pericardiocentesis, however the patient clinically improved following the procedure and there was visible improvement of the effusion on ultrasound. Referral to a facility with 24 hour monitoring was recommended, but ultimately declined. Tipper was clinically stable at the conclusion of the echocardiogram and pericardiocentesis.
Abnormal Echocardiogram Findings
The mitral valve is diffusely thickened especially the anterior leaflet with prolapse into the left atrial lumen during systole.
There is severe eccentric mitral regurgitation present.
There is severe left atrial enlargement (LA:Ao 3.0, normal under 1.6).
There is moderate left ventricular dilation (normalized LV diastolic diameter 2.0, normal under 1.7).
Mild right atrial and ventricular dilation (subjective).
Mild thickening of the tricuspid valve with mild TR and the velocity (3.8 m/s) is consistent with moderate pulmonary hypertension (57 mmHg).
There is a moderate pericardial effusion which does not appear to be causing tamponade. The echocardiogenic character of this effusion changes from hypoechogenic to having a more soft tissue appearance. This is consistent with an acute bleed and clot formation.
Diagnosis
Chronic degenerative valve disease causing severe mitral and mild tricuspid regurgitation. The LA is significantly dilated indicating a high risk for clinical signs going forward.
Moderate pulmonary hypertension is noted, which is likely secondary to chronic LA pressure elevation.
However there is a pericardial effusion likely secondary to left atrial rupture. Blood pressure should be assessed and if normal/high, therapy should be started such as an ACE inhibitor then amlodipine. The reduced systemic pressure will decrease the left atrial pressure and hence likelihood of continued left atrial breed.
Recommendations
Apart from blood pressure reduction, there is no specific treatment for left atrial rupture. Pericardiocentesis should only be performed if there is cardiac tamponade. It frequently recurs.
With this degree of left heart changes, the risk for spontaneous congestive heart failure is elevated and cardiac supportive medications are indicated as below. Pimobendan 0.2 – 0.3 mg/kg by mouth every 12 hours should be given to slow progression. Assessment of progression in the future will help predict long term outcome, however prognosis is guarded at this stage (late B2). Evidence for ACE inhibitors is equivocal at this stage. Unfortunately, the patient will always be at risk for recurrent CHF, development of arrhythmias/LA tear, syncope and/or sudden death in the future.
Close monitoring for development of associated clinical signs (development of increased breathing rate, labored breathing, exercise intolerance, cough or collapse episodes) is recommended. Monitoring of sleeping breathing rates is recommended as the best way to screen for CHF at home with less than 35 breaths/minute being normal.
Elective anesthesia is not advised, as there is high risk for complication such as heart failure.
Omega fatty acid supplementation and mild salt restriction may also be of some long term benefit.
A screening BP is recommended as hypertension makes mitral regurgitation worse.
A recheck echocardiogram is recommended in 4-6 months to screen for progression, sooner if clinical signs arise. If the results are similar, the recheck interval can be increased to 9 – 12 months.
Follow up
Tipper was started on Pimobendan (1.25mg orally twice daily), Furosemide (10mg orally twice daily), and Enalapril (2.5mg orally twice daily).
The week following Tipper’s echocardiogram, pericardiocentesis, and initiation of her cardiac medications,
Tipper’s owner reported she was feeling much better and acting her normal self.
Two months later, Tipper’s cardiac disease is still being managed, however ascites was noted again at that time, so her primary care veterinarian started her on Spironolactone in addition to her other cardiac medications. No signs of cardiac tamponade have been reported.
Special thanks to Montpelier Veterinary Hospital and Simon Swift, MA, VetMB, CertSAC, DipECVIM-CA (Cardiology), MRCVS with DVMStat for their collaboration on this case.
June's Case of the Month- 2022
Sonographer: Cary Sparkman, DVM
MALAKOPLAKIA, A RARE INFLAMMATORY CONDITION, IN A SUBLUMBAR MASS OF A 6 YEAR OLD CAT
PATIENT INFORMATION:
SPECIES/BREED: Feline/Domestic Short Hair
AGE: 6 years old
GENDER: MN
WEIGHT: 14 lbs
HISTORY:
The patient was presented for decreased appetite, lethargy, and occasional vomiting. The owner also reported diarrhea and leaking liquid feces. The patient has a chronic history of allergic dermatitis and otitis, which had been treated with oral cyclosporine for several months.
RADIOGRAPHS:
ABDOMINAL ULTRASOUND FINDINGS:
The bladder is moderately distended and turgid containing a moderate amount of echogenic luminal debris.
In the caudal abdomen dorsal to the bladder and colon is a very large (at least 3.5 x 4.8 trans, 3.2 x 5.6 sag) heterogenous hypoechoic mass which extends into the pelvic canal. Color flow is mild with Doppler color exam. Ultrasound guided fine needle aspirates were obtained.
CYTOLOGY FINDINGS:
Microscopic Description The slides are moderately to highly cellular and consist of a small to moderate amount of cellular debris, a proteinaceous background, few red blood cells and a nucleated cell population predominated by nondegenerate neutrophils with fewer but numerous macrophages that frequently exhibit leukophagocytosis. No microorganisms found after thorough search.
CYTOLOGIC DIAGNOSIS:
Most consistent with pyogranulomatous inflammation
Casey J. LeBlanc DVM, PhD, Diplomate, ACVP (Clinical Pathology)
Eastern VetPath
ADDITIONAL DIAGNOSTICS:
Auburn University Feline Infectious Peritonitis Virus mRNA: NEGATIVE
CT Scan:
There is a heterogenous soft tissue attenuating, variably contrast-enhancing mass extending through the pelvic canal into the caudal abdomen. The mass is causing significant cranial displacement of the urinary bladder. The mass is approximately 9-10 cm in sagittal length and 3-4 cm in cross-sectional height/width. The mass fills the entire cross-sectional diameter of the pelvic canal and appears to be causing severe ventral displacement of the colon, rectum and visible urethra. Mass margins are not well-defined relative to the hypaxial musculature ventral to the caudal lumbar, sacral and cranial coccygeal vertebrae.
Alaina Carr DVM, DACVR
Seattle Veterinary Specialists-Kirkland
Although it was unsure based on CT if complete excision could be achieved, the owners elected to attempt surgery because of the the cat’s increasing level of discomfort. Dysuria had been noted as well as tenesmus. The majority of the mass was removed and submitted for histopathology.
SURGERY REPORT:
A mass in the pelvic region just to the right of midline was carefully dissected from the right ureter and the iliac vessels. The mass was mildly friable and the surface vaguely appeared like the capsule of a lymph node. It was approximately 9 cm X 6 cm X 4 cm. The mass dove into epaxial muscle region. The mass was debunked removing at least 90% of what was present visibly and with palpation. The pelvic canal seemed to be free of obstruction.
HISTOPATHOLOGY FINDINGS:
Microscopic Findings: Sublumbar mass: Severe, dense, histiocytic inflammation consistent with malakoplakia.
COMMENTS FROM THE PATHOLOGIST:
Malakoplakia is a rare, reactive/inflammatory lesion most often associated with the presence of E. coli. It is caused by alterations in the degradative functions of macrophages following phagocytosis of bacteria (usually E. coli or Proteus) which results in a chronic inflammatory lesion that usually requires surgical excision for resolution. Since this disease is so rare, the diagnosis is somewhat presumptive and other well differentiated proliferations of histiocytes (such as a well-differentiated histiocytic sarcoma or a histiocytic proliferative disorder such as dendritic cell histiocytosis) were considered but are not favored.
Amy M. Boker, VMD, Diplomate ACVP
Antech
FOLLOW UP:
Malakoplakia is a rare condition in animals as well as humans. It is usually associated with the bladder, however, in this case, it was localized in the sub lumbar lymph node. It is a granulomatous disease characterized by impaired histiocytes that incompletely phagocytize bacteria, causing accumulation in macrophages.
This patient is doing very well after surgery with no other treatment required. The use of cyclosporine has been discontinued as this condition can sometimes be associated with immunosuppression.
Thank you to Drs. Watson and Sparkman at Noah’s Ark Veterinary Hospital for updates on this interesting case, as well as to Eastern VetPath, Antech, and Blue Pearl for the additional diagnostics!
May's Case of the Month- 2022
Sonographer: Kara Woody, DVM
Cystadenoma in Geriatric Feline
Patient Information:
Age: 14 years
Gender: Spayed Female
Breed: DSH
Species: Feline
History:
Patient presented with a history of hyporexia. Liver values were elevated on blood work and large mass associated with the liver was visualized on radiographs.
Ultrasonographic Findings:
There is a severely capsule deforming pedunculated hyperechoic loculated mass containing a single large anechoic cyst present in the distal right medial liver measuring 4.4x5.1cm. The rest of the liver is normal size, shape and echogenicity. The gallbladder is of normal size and shape and is clean. The common bile duct (1.5mm) and duodenal papilla (3.4mm) are WNL.
Abdominal Ultrasound Interpretation:
Right Liver Mass - the finding is severe - DDX: cystadenoma, well-differentiated cystadenocarcinoma or biliary adenocarcinoma. Hepatocellular carcinoma or hepatoma cannot be ruled-out without biopsy.
Large cyst associated with loculated hyperechoic right liver mass.
Treatment:
The rdvm performed a complete excisional biopsy of the liver mass.
Cystadenoma during surgical removal
Histopathology Results:
Biliary Cystadenoma with clean margins
Outcome:
The patient made a full recovery with normalization of liver values at the 1 month recheck and complete resolution of clinical signs.
Patient recovering after surgery!
Discussion
These masses are generally non-malignant/benign but can create clinical signs based on their shear size and space-occupying nature. Where possible, surgical resection is the best therapy for these lesions. Sometimes, these masses are close to the hepatic vasculature and/or biliary system which can make surgical resection difficult. Fortunately, in this case, the mass was present on the distal right liver so it was amenable to surgical resection.
Thank you to Hope Animal Hospital and Dr. Faiz Ahmad for providing surgical pictures and collaborating with us on this interesting case!
April's Case of the Month- 2022
Sonographer: Anne Desrochers, DVM DACVIM
Intestinal obstruction in a cat
Patient Information:
Species: Feline
Breed: Maine Coon Mix
Gender: Neutered Male
Age: 13 years old
History:
The patient presented for 24-hour history of inappetence, vomiting bile, not defecating or urinating. Bloodwork revealed leukocytosis. Abdominal radiographs showed gas-filled segments of gastrointestinal tract but no obvious foreign body.
Ultrasound Findings:
One large partially to completely obstructive cylindric hyperechoic structure casting a strong acoustic shadow was seen in a segment of jejunum consistent with a foreign body measuring several centimeters in length. The wall of the involved jejunum was moderately thickened (3.7mm), hypoechoic and lack normal wall layering. The oral segments of jejunum were moderately distended with gas and fluidy ingesta and were hypomotile to amotile. The aboral segment was empty. In addition, many loops of small intestine were mildly to moderately thickened (max: 3.7mm) with prominent disproportionate thickening of the muscularis layers. The mesentery was diffusely hyperechoic and a scant amount of free anechoic peritoneal effusion was detected.
Image 1. The jejunum was distended by a structure with a strong echogenic interface and clean distal acoustic shadowing (FB). Notice the thickening and loss of layering of the involved jejunal wall. The intestinal loop proximal to the obstructing material was distended with gas and fluid (arrow). Three empty small intestinal loops are visible in the upper portion of the image showing selective thickening of the muscularis layer (*)
Surgery:
Exploratory laparotomy was performed and large trichobezoar obstructing the mid jejunum was removed via enterotomy. Multiple biopsies were obtained for histopathologic evaluation.
Image #2. Trichobezoar
Histopathologic diagnosis:
findings consistent with small cell lymphoma invading the mucosa, submucosa and muscularis layers of the duodenum, jejunum and ileum.
Outcome:
Besides initial inappetence, the patient recovered uneventfully from surgery. The pet was referred to the oncology service and was started on a tapering dose of Prednisolone, weekly vitamin B12 injection and Chlorambucil and has been progressing well to date.
Secondary disturbances of the digestive motility pattern by the infiltrative neoplasia likely contributed to the delayed intestinal transit and hair ball formation in this case. It is suggested that biopsy specimens be obtained at time of surgery in patients suffering from obstructive hairballs to detect potential causes of gastrointestinal dysmotility.
Special thanks to Drs. Myzie and Taylor and the staff at
Animal Medical Center of Loudoun – Ashburn Farms as well as
The Oncology Service of Leesburg for their help with this case.
March's Case of the Month- 2022
Sonographer: Tyler Anderson, DVM
Sonographic Findings of Colonic Carcinoma with Regional Lymph Node Metastasis: A Case of the Month March 2022
Patient Information:
Age: 10 years
Gender: Spayed Female
Species: Feline
Breed: DSH
History:
An abdominal ultrasound was recommended due to a one month history of persistent soft stool and hematochezia. No vomiting or changes in appetite were noted by the owner. Patient was treated with metronidazole with no significant improvement. Patient also has a history of Grade II/VI murmur.
Image Interpretation:
Abdominal sonographic findings
Segments of jejunum are prominent and mildly thickened measuring 2.7 to 3.1 mm (normal wall thickness ~2.2-2.5mm, > 2.8mm abnormal Norsworthy/Estep et. al. JAVMA, Vol 243, No. 10, November 15, 2013). Normal layer proportionality is maintained without excessive thickening of the muscularis layer.
An annular, hypoechoic, vascular mass is seen in descending colon, measuring ~ 11.1mm in wall thickness. The mass has near complete loss of wall layering distinction.
The jejunal lymph nodes are moderately to severely enlarged with rounded shape having homogenous hypoechoic echogenicity, measuring ~ 1.4cm in thickness.
Other findings include a trace amount of anechoic ascites and chronic degenerative changes to both kidneys.
Distal Colonic Mass with severe wall thickening and near complete loss of normal wall layering distinction. Fecal contents casting a shadow can be seen within the lumen.
A moderately to severely enlarged and hypoechoic jejunal lymph node. Color doppler is utilized to assess vascularity prior to fine needle biopsy.
Cytologic interpretation provided by Eastern Vet Path - Casey J. LeBlanc DVM, PhD, Diplomate, ACVP (Clinical Pathology)
Diagnosis and Sonographic Analysis:
Sedated fine needle colonic and regional lymph node biopsies were obtained for cytologic review. Both sites revealed an epithelial tumor with necrosis most consistent with metastatic Carcinoma.
Special Thanks to Arlington Animal Hospital for the interesting case and follow-up!
February's Case of the Month- 2022
Sonographer: Meredith Adams, DVM
February 2022 Case of the Month.
Patient Information:
Age: 12 years
Gender: Castrated Male
Breed: Shepherd Mix
Weight: 57 pounds
History:
Presented for abdominal ultrasound to evaluate for underlying cause of intermittent decreased appetite and a possible abdominal mass. Popliteal lymph nodes were also noted to be mildly enlarged on physical examination.
Abdominal ultrasound findings:
Liver:Normal size with rounded shape and hypoechoic echogenicity. No focal lesions are appreciated.
Spleen: Diffusely enlarged measuring 2.8cm having scalloped shape and a miliary pattern of hypoechoic micronodules throughout.
Stomach: The stomach is empty and collapsed with diffusely thickened walls (11.0mm)
Lymph Nodes: Multiple mesenteric lymph nodes are moderately enlarged (~1.4cm depth) with rounded shape having homogenous hypoechoic echogenicity.
The medial iliac lymph nodes and inguinal lymph nodes are severely enlarged (medial iliacs Lt/Rt 1.2/2.3cm; right inguinal 0.9cm) with rounded shape having homogenous hypoechoic echogenicity.
Other lymph node populations throughout the abdomen are also enlarged, rounded, with homogenous hypoechoic echogenicity.
Mesentery: diffusely hyperechoic throughout the abdomen
Differentials:
Liver - the findings are moderate - DDx:
a) Common: Hepatitis (acute or active): Vacuolar hepatopathy, Passive congestion (e.g., dilated hepatic veins and CVC), Cholangiohepatitis/cholangitis (acute or active), Neoplasia (e.g., lymphoma, sarcoma, histiocytic neoplasia, or mast cell disease)
b) Less Common: Immune-mediated hemolytic anemia, Leptospirosis, Histoplasmosis, Amyloidosis, Leukemia
Stomach wall thickening - the findings are moderate - DDx: adenocarcinoma vs. infiltrative neoplasia (lymphosarcoma) vs. leiomyosarcoma vs. leiomyoma vs. benign mucinous hypertrophy or gastric ulcer.
Spleen - the findings are moderate - DDx: extramedullary hematopoiesis (EMH) vs. infiltrative neoplasia vs. benign nodular regeneration
Lymph nodes - the findings are severe - DDx: infiltrative neoplasia (lymphoma vs. mast cell vs. other) vs. IBD vs. infection vs. reaction vs. metastatic neoplasia
Mesentery - the findings are moderate - DDx: peritonitis - inflammation vs. paraneoplastic reaction vs. infectious vs. fibrosis vs. other.
Additional Diagnostics:
Ultrasound guided fine needle aspirates of the right medial iliac lymph node and the spleen were obtained and submitted to Eastern Vet Path for analysis
Cytology:
Microscopic Description
The slides from the two locations appear very similar, are highly cellular, and consist of few to numerous red blood cells and a nucleated cell population predominated by large immature lymphocytes, with few small lymphocytes, and occasional neutrophils. The slides from the spleen also consist of few aggregates of splenic stroma and few hematopoietic precursors. The large lymphocytes consist of a small amount of basophilic cytoplasm, a perinuclear clear area, and a large round nucleus with a finely-stippled chromatin pattern. Occasional mitotic figures are noted. The background consists of many lymphoglandular bodies and occasional free nuclei.
Diagnosis:
Spleen: High-grade lymphoma definitive (100% confidence)
Right medial iliac lymph node: High-grade lymphoma definitive (100% confidence)
Treatment Options:
Referral for oncology consultation was recommended for optimal treatment plan. Alternatively, for immunophenotyping (T vs B cell), ICC staining of slides could be performed and/or a lymphoma chemotherapy protocol could be initiated. Palliative treatment options could also be considered based on the patient's clinical condition.
January's Case of the Month- 2022
Sonographer: Emily Evans, BVM&S
Acute hypersensitivity Reaction with Anaphylaxis of Unknown Cause.
PATIENT INFORMATION:
Age: ~2 year old
Gender: Male neutered
Species: Canine
Breed: Chihuahua Mix
Weight: 15lbs
HISTORY:
Previously healthy and fully vaccinated. Presented acutely at home foaming at the mouth with grey mucous membranes and weakness. No cutaneous signs noted. No history of toxin ingestion, envenomation, medications, trauma or illness.
INITIAL ULTRASOUND ANALYSIS:
Mild-moderate free fluid in the abdomen. Severely thickened isoechoic gallbladder wall.
ADDITIONAL DIAGNOSTICS:
SERIAL ULTRASOUNDS IMAGES:
Gallbladder
Pancreas
SELECT CLIPS:
Image 1: Marked pancreatic change 2-3 hours after initial presentation. Note “tiger stripe” appearance secondary to edema.
Image 2: Abdominal free fluid at presentation.
DIAGNOSIS:
Anaphylaxis of unknown origin
CASE OUTCOME:
Patient was treated with steroids, diphenhydramine, metronidazole and fluid therapy. After 36 hours the patient returned to normal.
PROGNOSIS/DISCUSSION:
It has been found that elevated ALT and gallbladder wall changes are significantly associated with anaphylaxis in dogs with acute hypersensitivity reactions. Gallbladder changes alone are not pathognomonic for anaphylaxis. Other potential causes of gallbladder changes include right-sided congestive heart failure and should be ruled out.
Spontaneous abdominal effusions are commonly associated with anaphylaxis.
References:
*Quantz JE, Miles MS, Reed AL, White GA. Elevation of alanine transaminase and gallbladder wall abnormalities as biomarkers of anaphylaxis in canine hypersensitivity patients. J Vet Emerg Crit Care (San Antonio). 2009 Dec;19(6):536-44. doi: 10.1111/j.1476-4431.2009.00474.x. PMID: 20017759.
Hnatusko AL, Gicking JC, Lisciandro GR. Anaphylaxis-related hemoperitoneum in 11 dogs. J Vet Emerg Crit Care (San Antonio). 2021 Jan;31(1):80-85. doi: 10.1111/vec.13017. Epub 2020 Oct 29. PMID: 33118683.
Summers AM, Culler C, Cooper E. Spontaneous abdominal effusion in dogs with presumed anaphylaxis. J Vet Emerg Crit Care (San Antonio). 2021 Jul;31(4):483-489. doi: 10.1111/vec.13070. Epub 2021 Apr 29. PMID: 33913584.
December's Case of the Month!
Sonographer: Cary Sparkman, DVM
Decembers Case of the Month- Bilateral Adrenomegaly in a Dog
Patient Information:
Age: 11 years old
Gender: Spayed Female
Breed: Border Collie Mix
Weight: 62.5 lbs
History:
Several weeks duration of intermittent decreased appetite, lethargy, and pu/pd. Labwork showed a mild non regenerative anemia and mild azotemia. A urine cortisol creatinine ratio was not suggestive of hyperadrenocorticism. The patient had recently been treated for a fever and a UTI. Amlodipine was recently started for treatment of hypertension.
Abdominal Ultrasound Findings:
Adrenal Glands
The left adrenal is very enlarged (Lft cd,cr - 20,13 mm), plump in shape, and hyperechoic with multiple partially mineralized nodules.
The right adrenal is very enlarged (Rt cd,cr - 22,19 mm), irregular in shape and mineralized. Invastion into the caudal vena cava is suspected and Doppler blood flow deficits within the caudal vena cava are noted.
Other sonographic findings:
Multiple ill-defined splenic nodules
Mild to moderate diffuse hepatopathy
Chronic renal changes
Biliary debris
Interpretation:
Bilateral adrenomegaly is most commonly seen in dogs associated with pituitary dependent hyperadrenocorticism, however, this patient’s adrenal glands demonstrated multiple abnormal features. The general criteria of malignancy associated with adrenal tumors are a measurement of >1.5 to 2 cm in width, mineralization, and vascular invasion, all of which were visualized in this patient.
Bilateral adrenal tumors are uncommon in dogs, but can occur. Concurrent pituitary dependent AND adrenal dependent hyperadrenocorticism can occur and is also uncommon. Given that this patient’s UCCR was negative, functional adrenal masses are less likely. Other differentials include inactive adrenocortical neoplasia, pheochromocytoma, or metastatic disease from neoplasia elsewhere.
Outcome:
Because of bilateral involvement, surgery was not a feasible option. A University of Tennessee adrenal profile was performed and was abnormal for all hormones with the exception of cortisol. The patient is currently doing well and managed on melatonin and lignans with periodic monitoring of UAs for recurrent UTIs
The left adrenal is very enlarged (Lft cd,cr - 20,13 mm), plump in shape, and hyperechoic with multiple partially mineralized nodules.
The right adrenal is very enlarged (Rt cd,cr - 22,19 mm), irregular in shape and mineralized. Invastion into the caudal vena cava is suspected and Doppler blood flow deficits within the caudal vena cava are noted.
Special thank you to Farmers Veterinary Hospital and DVM Stat IMED for information and follow up on this case.
November's Case of the Month!
Sonographer: Lauren Pike, DVM
November 2021 Case of the Month - Emphysematous Cystitis in an Intact Male Dog
Patient Information:
Age: 12 years
Sex: Male
Breed: Shiba Inu
History:
A 12 year old intact male Shiba Inu presented for ultrasound following a several month history of inappropriate urination as well as decreased appetite. Urinalysis showed glucosuria, though no hyperglycemia was reported.
Ultrasound Findings:
The bladder is moderately distended with anechoic urine and there is a moderate amount of gas within the superficial bladder lumen and bladder wall; however, the bladder is of relatively normal contour and thickness. Also noted are occasional uroliths measuring up to ~0.5 cm within the dependent bladder.
Interpretation:
Gas within the bladder wall and bladder lumen is consistent with emphysematous cystitis. This is a rare condition which is often associated with comorbidities such as impaired immune system (hyperadrenocorticism, long-term corticosteroid therapy, etc), cystolithiasis, neurologic bladder, chronic UTI, and diabetes mellitus. Interestingly, one study does not show any gender predisposition, though a more typical UTI would be expected to be found more frequently in females.
E. coli is the most common isolate in this condition, and is what was cultured from this patient’s urine. This bacteria ferments glucose and lactate into gases such as CO2, O2, and H2, which would explain the role of diabetes mellitus or other glycosuric conditions in the development of emphysematous cystitis. In the case of our patient, glucosuria was despite the absence of hyperglycemia. Glucosuria in the absence of hyperglycemia is suspicious for proximal renal tubular disease/injury. This may include Fanconi syndrome, jerky treat exposure, pyelonephritis, Leptospirosis, NSAIDs, or toxins.
Treatment:
The patient is currently being treated for his emphysemtous cystitis with enrofloxacin, and is responding well so far.
Reasonable workup of his glucosuria would include ruling out any exposure to jerky treats of any kind, then consider Leptospirosis testing and a Fanconi panel.
References:
Lippi I, Mannucci T, Santa DD, Barella G, Oranges M, Citi S. Emphysematous cystitis: Retrospective evaluation of predisposing factors and ultrasound features in 36 dogs and 2 cats. Can Vet J. 2019;60(5):514-518. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6463776/
Gas within the bladder wall and bladder lumen is consistent with emphysematous cystitis.
Thank you to Ohana Veterinary Care for collaborating with us on this interesting case.
October's Case of the Month
Sonographer: Kara Woody, DVM
Multiple Neoplasias in a Geriatric Canine
Patient Information:
Age: 14
Gender: Neutered Male
Breed: Terrier Mix
Species: Canine
History:
Patient had history of apocrine gland anal sac adenocarcinoma in September 2020. He recently had a decrease in appetite and increase in coughing. Liver values were newly elevated. Ultrasound was requested to check for any metastasis.
Ultrasonographic Findings:
The liver was normal size and mildly irregularly contoured with a coarse hypoechoic echogenicity. The periportal lymph nodes were prominent (1.4x2.1cm) and rounded with a heterogenous hypoechoic echogenicity. Additionally, the spleen was noted to have multiple ill-defined small (<1.0cm diameter) homogenous hypoechoic nodules throughout the parenchyma.
Abdominal Ultrasound Interpretation:
Liver - the findings are moderate- DDx:
a) Common: Hepatitis (acute or active): Vacuolar hepatopathy, Passive congestion (e.g., dilated hepatic veins and CVC), Cholangiohepatitis/cholangitis (acute or active), Neoplasia (e.g., lymphoma, sarcoma, histiocytic neoplasia, or mast cell disease)
b) Less Common: Immune-mediated hemolytic anemia, Leptospirosis, Histoplasmosis, Amyloidosis, Leukemia
Lymph nodes - the findings are moderate - DDx: infiltrative neoplasia (lymphoma vs. mast cell vs. other) vs. reaction vs infection vs. metastatic neoplasia
Spleen nodules- the findings are mild - DDx: extramedullary hematopoiesis (EMH) vs. infiltrative neoplasia vs. benign nodular regeneration vs reactive nodules
Additional Diagnostics:
Ultrasound guided fine needle aspirate of the liver was performed and submitted to Eastern VetPath for analysis.
Cytology Findings:
Microscopic findings:
The slides are moderately cellular and consist of many red blood cells and a nucleated cell population predominated by intermediate to large immature lymphocytes, other leukocytes in proportions consistent with peripheral blood, and several clusters of uniform and well-differentiated hepatocytes. The intermediate to large lymphocytes consist of a small amount of basophilic cytoplasm and an intermediate to large round nucleus with a finely-stippled chromatin pattern. Occasional mitotic figures are noted. The background consists of many lymphoglandular bodies and occasional free nuclei.
Diagnosis:
High-grade lymphoma-100% confidence
Treatment:
Treatment options included referral to oncologist for chemotherapy, palliative corticosteroids or humane euthanasia. Sadly, our patient’s condition rapidly deteriorated and he was euthanized.
Discussion:
While initially metastasis of previously diagnosed apocrine gland anal sac adenocarcinoma was clinically suspected, this patient had developed an additional unrelated neoplasia. Unfortunately, this can occur particularly in our geriatric patients. It is important to consider additional neoplasias as part of our differentials.
Sonographer: Kara Woody, DVM
Hypoechoic liver with prominent hyperechoic perivascular markings and an irregular margin.
A rounded heterogenous hypoechoic periportal lymph node.
Liver cytology: A small cluster of hepatocytes surrounded by several intermediate to large lymphocytes.
Thank you to Kindness Animal Hospital and Eastern VetPath for collaborating with us on this interesting case.
September's Case of the Month
Sonographer: Anne Desrochers, DVM DACVIM
Intestinal Intussusception in a cat
Patient Information:
Age: 3-month-old
Species: Feline
Breed: Domestic short hair
Gender: Female
History:
Previously healthy kitten. The patient presented with a 2-day history of vomiting, progressive lethargy and anorexia. A thickened loop of intestine was felt on palpation. Abdominal radiographs were unremarkable.
In one study of 20 affected cats with intestinal intussusception, 10 were <1 year of age and 9 were ≥6 years of age. Siamese cats were overrepresented. No sex predisposition was noted. A wide range of acute and chronic gastrointestinal signs have been reported. Abdominal ultrasound is the preferred method of diagnosis.
Ultrasound Findings:
Segments of small intestine (intussusceptum) were seen invaginated within the colon (intussuscipiens) in the right cranial abdominal quadrant. The cecum and a portion of the mesentery were seen adjacent to the intussusceptum within the lumen of the intussuscipiens. The walls of the affected colon and small intestine appeared moderately thickened and hypoechoic with indistinct wall layering most likely due to congestion and edema.
Image 1 (found below). Transverse ultrasound image of a typical target-like mass consistent with an intussusception using a high frequency probe. Multiple loops of small intestine (arrows) were located eccentrically within the colon (cross) along with the cecum (arrowhead) and a portion of the mesentery (asterisk).
Surgery:
The patient was referred for emergency surgery. The intussusception was identified and reduced by manual manipulation. The ileum was markedly bruised with serosal tearing, but no intestinal leakage was appreciated. The remaining small intestine appeared normal and no foreign material or mass was identified. Empirical deworming with Fenbendazole was performed following surgery.
Although spontaneous reduction can occur, most intussusceptions require surgical reduction. Once reduced, involved intestines are evaluated for perforations and viability. Intestinal resection and anastomosis may be necessary in some cases. Enteroplication (i.e. entero-enteropexy) can be performed to prevent recurrence but this procedure is controversial due to a complication rate approaching 20%.
Outcome:
The exact cause of the intussusception could not be clearly established in this case. The patient recovered uneventfully from surgery and has been growing normally without evidence of recurrence to date.
In one report, 10/13 cats that underwent corrective surgery survived to discharge. If the underlying cause of the intussusception is not adequately addressed, risk of recurrence increases. Any condition responsible for hyperperistalsis can predispose to an intussusception. Causes include intestinal parasitism, foreign bodies, acute enteritis (e.g. viral, bacterial), intestinal neoplasia, prior abdominal surgery, inflammatory bowel disease, metabolic disorders, etc. The intussusception can also be idiopathic.
Barreau P: Intussuscpetion: Diagnosis and Treatment. World Small Animal Veterinary Association World Congress Proceedings 2008.
Burkitt JM, Drobatz KJ, Saunders HM, et al: Signalment, history and outcome of cast with gastrointestinal tract intussusception: 20 cases (1986-200). J Am Vet Med Assoc 2009 Vol 234 (6) pp. 771-6.
Sonographer: Anne Desrochers, DVM DACVIM
Image 1 . Transverse ultrasound image of a typical target-like mass consistent with an intussusception using a high frequency probe. Multiple loops of small intestine (arrows) were located eccentrically within the colon (cross) along with the cecum (arrowhead) and a portion of the mesentery (asterisk).
Special thanks to the staff at Adam’s Mill Veterinary Hospital for their help with this case.
August's Case of the Month
Sonographer: Tyler Anderson, DVM
Sonographic Findings of a Congenital Pericardial-Peritoneal Diaphragmatic Hernia in a 6 month old Ragdoll. Case of the Month August 2021.
Patient Information:
Age: 6 months
Gender: Female (intact)
Species: Feline
History:
An abdominal ultrasound was recommended due to a persistently elevated ALT/ALKP (ALT: 915 U/L; ALKP 195 U/L). Although the patient’s ALT improved mildly with 10 days of metronidazole, repeat lab work revealed persistently elevated ALT/ALKP. The patient had no GI symptoms or signs of respiratory distress. Pre and post-prandial bile acids were WNL. AUS was recommended prior to spay to help determine anesthetic risks.
Image Interpretation and Analysis:
Abdominal sonographic findings:
A defect in the diaphragm was seen along the medial aspect near the right-side of the liver creating a “bulge” of liver parenchyma within the thoracic cavity.
Upon, closer examination the gall-bladder was also seen prolapsed into the thorax.
The left liver, stomach, spleen, and small bowel remained within the abdominal cavity. No effusions were observed.
In one view, liver parenchyma can be seen in the intercostal space abutting the heart.
The patient was referred for to VSC for a surgical consultation to repair the hernia and OHE. Upon surgery, a pericardial-peritoneal diaphragmatic hernia was present. The herniated right liver and gallbladder were reduced back into the abdomen and the hernia was repaired. OHE was also performed at this time.
A defect in the diaphragm was seen along the medial aspect near the right-side of the liver creating a “bulge” of liver parenchyma within the thoracic cavity.
Upon, closer examination the gall-bladder was also seen prolapsed into the thorax.
The left liver, stomach, spleen, and small bowel remained within the abdominal cavity. No effusions were observed.
Special Thanks to City Paws Animal Hospital for the follow-up and interesting case.
July's Case of the Month
Sonographer: Emily Evans, BVM&S
Unexpected finding in dog with new asymptomatic III/VI murmur
PATIENT INFORMATION:
Age: 11year
Gender: Female Spayed
Species: Canine
Breed: Border Collie Mix
Weight: 40.6lbs
HISTORY:
New III/VI murmur noted at annual exam. No exercise intolerance, cough, or other signs of cardiac disease.
INITIAL ECHOCARDIOGRAM ANALYSIS:
A moderate sized, pedunculated mass was identified within the right ventricular outflow(RVOT) just below the pulmonic valve. Additionally, mild chronic degenerative valve disease (stage B1) resulting in mild mitral regurgitation and tricuspid regurgitation.
RECHECK ECHOCARDIOGRAM ANALYSIS(11 months post initial diagnosis):
Minimal change in the RVOT mass(suspected ectopic thyroid tumor). (25 x 19mm; previously 25 x 18mm) Increasing RVOT velocities (increased to 2.4 m/s from 1.8m/)) suggesting the development of mild obstruction.
ADDITIONAL DIAGNOSTICS:
Abdominal ultrasound was performed a month after the initial echocardiogram. Single ill-defined nodule(likely benign change) noted in the spleen and unilateral adrenomegaly identified.
DIAGNOSIS:
RVOT neoplasia.
Though uncommon in general, cardiac masses are typically found to be hemangiosarcoma, aortic body tumours ( most commonly chemodectoma), lymphoma and ectopic thyroid carcinomas. Numerous other cardiac tumors(including myxoma, sarcomas and metastatic lesions) have been described in case reports but are rare.
Ectopic thyroid tumors are often identified within the RVOT and are associated with the embryologic development of thyroid and right ventricular outflow tract.
CASE OUTCOME:
The patient continues to do well clinically with no clinical signs beyond a cardiac murmur. A monitoring echocardiogram is upcoming. No therapies have been initiated and the owner has elected monitoring at this time.
PROGNOSIS/DISCUSSION:
Given the location, ectopic thyroid carcinoma was initially suspected but minimal progression has opened the possibility of other tumor types. A biopsy of the mass is needed for a definitive diagnosis.
The expected prognosis as the mass grows is poor as RVOT obstruction will eventually develop which will lead to right sided congestive heart failure. Minimal change over 11 months hopefully means this is a slow growing tumor type and the time to onset of right heart failure will be long.
Additional therapeutic options could include radiation therapy to slow tumor growth or reduce tumor size of the mass and stenting the RV outflow tract when needed.
Image 1: RVOT mass at initial echocardiogram
Image 2: RVOT tract mass 11 months post diagnosis. Minimal change noted in mass size.
Video 1: RVOT color flow doppler indicating partial outflow obstruction.
Video 2: Right ventricular outflow tract (RVOT) Mass moving within the RVOT.
A special thank you to Cardinal Animal Hospital and DVMSTAT Consulting for collaborating with us on this interesting case.
June's Case of the Month
Sonographer: Lauren Pike, DVM
A Diaphragmatic Hernia in a Cat
Patient Information
Age: 4 years old
Gender: Spayed Female
Species: Feline
Breed: Domestic Medium Hair
History:
A 4 year old female spayed domestic Medium hair cat presented with a 1 month history of vomiting and decreased appetite. She was not known to chew or ingest inappropriate items.
Ultrasound Findings:
No hepatic tissue is noted left cranial abdomen. It appears that the left liver lobes are deviated to the right cranial abdomen, and the right liver lobes and gallbladder are appreciated in the mid to cranial right thorax (the gallbladder is of normal size, shape, and is clean).
Many well-defined, homogenous hyperechoic nodules measuring 0.6x0.5 cm are noted throughout the hepatic tissue within the thorax; no focal lesions are noted within the intra-abdominal liver. The visible liver retains normal shape and echogenicity; size could not be confidently evaluated.
Image Interpretation:
The findings are consistent with a diaphragmatic hernia; peritoneopericardial diaphragmatic hernia is not suspected.
Discussion:
A diaphragmatic hernia is the dislocation of abdominal contents into the thorax through a defect in the diaphragm. These can be acquired (trauma) or congenital (with PPDH being more common in congenital cases) in origin. Radiographs may be enough to diagnose a diaphragmatic hernia, though in some cases the degree of pleural effusion may prevent visualization of abdominal viscera within the thorax. Furthermore, in this case only a small section of the stomach and pylorus are thought to be involved, and if only liver were seen within the thorax, further diagnostics would have been required to confirm this as the cause of the patient's vomiting. In addition to ultrasound, contrast radiography or CT/MRI may be considered when necessary.
Possible sequalae include respiratory distress due to mass effect of involved organs and pleural effusion, entrapment and necrosis of viscera, tension gastrothorax (which can be acutely life-threatening), and poor intestinal function. PPDH may produce no signs (if a larger hernia which allows organs to move back and forth freely), or may result in reduced cardiac function, pericardial effusion, and arrhythmias. Clinical signs vary depending on severity and may include respiratory distress and other respiratory signs, cardiac signs such as arrhythmias, pale or cyanotic mucous membranes, as well as GI signs like vomiting, diarrhea, weight loss, inappetence, and even shock or acute death. With congenital disease, clinical signs may not be noted until later in life.
Surgery is the required treatment for diaphragmatic hernias. If necessary, the pet should be stabilized prior, and prophylactic antibiotics may be considered if there is herniation of the liver, due to potential for toxin release if there has been hepatic strangulation or vascular compromise. Possible surgical complications include increased intra-abdominal pressure if the DH is chronic, or pulmonary edema secondary to re-expansion. Bella the cat has surgery scheduled in July.
The liver (with multifocal nodules which are likely fatty deposits) and gallbladder are seen between the shadows caused between two ribs. The right liver is located within the cranial right thorax.
The liver (left) and heart (right) are seen adjacent to each other. The liver does not appear to be within the pericardium, so peritoneopericardial diaphragmatic hernia is not suspected.
Special thanks to Old Bridge Veterinary Hospital for allowing us to collaborate on this case.
May's Case of the Month!
Sonographer: Kara Woody, DVM
Pulmonary Chondrosarcoma In a Newfoundland
Patient Information:
Age: 5 years
Gender: Neutered Male
Species: Canine
Breed: Newfoundland
History:
Patient presented to the emergency clinic for vomiting and diarrhea. Chest radiographs were taken as part of diagnostics and 2 rounded soft tissue nodules were visualized in the caudal portion of the left cranial lung lobe measuring ~2.5 and 1.7cm
Ultrasonographic Findings:
There was a well circumscribed hypoechoic nodule in the left mid lung field measuring 0.8x0.7cm. Around this nodule there was a "shred sign" noted. The rest of the lung field displayed normal A-lines.
Abdominal Ultrasound Interpretation:
Lung nodule- the findings were moderate and indicated either primary or metastatic pulmonary neoplasia (lung abscess, benign lesion, parasitism or fungal infection cannot be ruled out without biopsy).
Additional Diagnostics:
A CT was performed which confirmed an isolated cluster of small nodules in the caudal portion of the left cranial lung lobe. The rest of the lung lobes were normal. An ultrasound guided fine needle aspirate was performed on the peripherally visualized nodule and submitted to Eastern VetPath.
Cytology Findings:
The slides are moderately cellular and consist of a few red blood cells and nucleated cell population predominated by individual round to irregularly shaped cells with very few scattered leukocytes. The round to irregularly shaped cells have a cytoplasm and an eccentric, round to oval nuclei, and have a finely stippled chromatin pattern and 1-3 prominent nucleoli. Anisokaryosis is moderate. The cells are surrounded by a very lkarge amount of think pink matrix.
Diagnosis:
Highly suspect chondrosarcoma.
Treatment:
The patient was referred to a boarded surgeon for lung lobectomy of the caudal aspect of the left cranial lung lobe. At the time of surgery, a firm, pale purple, nodular 3.5cm mass was present on the periphery of the caudal aspect of the left cranial lung lobe. Histopathology confirmed a low grade chondrosarcoma that was completely excised. The patient is doing great following surgery and will follow-up with oncology as appropriate.
Discussion:
While the lungs are a common location for metastatic chondrosarcoma, there were no other primary sources found for this tumor in our patient. There is very little data in the literature in humans or animals on primary chondrosarcoma within the pulmonary tissue; however it has been reported in both humans and dogs. It is currently believed that prognosis is good with lung lobectomy if the mass is discovered early and can be completely resected and is low grade.
This case also illustrated how only peripheral lung lesions can be visualized with ultrasound techniques. This is due to air interference, which effectively "blocks" visualization of lesions present within the deep lung tissue. Only a small portion of this nodular mass was seen on ultrasound. Fortunately, in this case, the area was large enough to obtain a diagnostic cytology sample with ultrasound guidance.
A small hypoechoic nodule is seen in the mid aspect of the left lung field.
CT image of cluster of nodules within the left lung field.
A few round to irregularly shaped cells exhibiting anisokaryosis and prominent nucleoli, surrounded by abundant pink matrix.
Thank you to The Oncology Service and Eastern VetPath for collaborating with us on this interesting case.
April's Case of the Month
Sonographer: Anne Desrochers, DVM DACVIM
Cervical Mass in a Dog.
Patient Information:
Age: 10-year old
Gender: Neutered Male
Species: Canine
Breed: Saluki
History and clinical findings:
The owner noticed an area of swelling on right proximo-lateral cervical region one week prior to presentation which had tripled in size and was painful on palpation. The patient had a right thyroid gland carcinoma removed 3 months prior to presentation.
Ultrasound Interpretation:
The right mandibular salivary gland (MSG) was moderately enlarged (2.3x3.7cm in diameter) and had a slightly heterogenous hyperechoic echogenicity when compared to the left MSG. A well-defined thin-walled area containing anechoic fluid and flocculent hyperechoic particles/debris was seen extending from the right MSG measuring 2.1x5.2cm in diameter. No evidence of sialoliths was detected. The soft tissue surrounding the affected gland was diffusely moderately hyperechoic and contained a few small anechoic fluid pockets (edema). The visible retropharyngeal lymphnodes and cervical bone structures had a normal sonographic appearance.
Sampling:
Ultrasound-guided fine-needle biopsies of the affected gland and fluid samples were collected under sedation and submitted for cytology and fluid analysis.
Diagnosis:
Epithelial cell proliferation with mild atypia; mixed, predominantly neutrophilic inflammation. Viscous fluid with mixed macrophagic, neutrophilic, and lymphocytic inflammation; suspect inflamed salivary mucocele. The prior history of thyroid carcinoma and the hyperplastic epithelial proliferation were concerning for neoplasia, although some of the epithelial atypia could have been dysplastic changes secondary to the significant inflammatory process present.
Case management:
Since the patient was experiencing discomfort, surgical exploration and removal was performed. Histopathology evaluation revealed findings consistent with salivary gland mucocele formation without evidence of underlying infection or neoplasia. The patient made an uneventful and complete recovery.
Image #1: The owner noticed an area of swelling on right proximo-lateral cervical region one week prior to presentation which had tripled in size and was painful on palpation.
Image #2: A well-demarcated, fluid-filled structure is seen expending from the margin of the right mandibular salivary gland. The cystic lesion contains hyperechoic sedimenting debris.
Image #3: Aggregate of epithelial cells some displaying mild atypia.
Special thanks to Dr. Mitchell and the staff at Blue Ridge Veterinary Associates and pathologists at IDEXX for their help with this case.
March's Case of the Month 2021
Sonographer: Tyler Anderson, DVM
Sonographic Findings of a Radiolucent Obstructive Foreign Object in a Sphynx.
Patient Information:
Age: 6 years
Gender: Male Neutered
Species: Feline
History:
An abdominal ultrasound was recommended due to a recent onset of reduced appetite and vomiting. Owner reported a possible missing child’s toy. Radiographs were performed with no foreign material noted. AUS was performed prior to exploratory laparotomy.
Image Interpretation and Analysis:
Abdominal sonographic findings:
An approximate ~ 4.0cm hypoechoic foreign object with hyperechoic margins was seen in the jejunal lumen. The object had characteristics of a small animal, having discernible feet, hindlimbs, tail, abdomen, and a tail. No head could be seen. Unlike most foreign objects, this structure had no acoustic shadow that is typically seen with foreign material.
Other sonographic abnormalities included irritated/spastic jejunal segments that were moderately corrugated, and hyperechoic mesentery suggestive of mild peritonitis with no evidence of ascites.
Surgery was recommended to remove the foreign material, assess bowel integrity, and abdominal lavage.
Post-surgical evaluation of the foreign object revealed a foam-like dinosaur with a missing head that likely passed without obstruction. Upon follow-up with the owner, a bath-bomb had recently been used that contained various floating dinosaurs.
Radiographs were performed with no foreign material noted.
An hypoechoic foreign object with hyperechoic margins was seen in the jejunal lumen. The object had characteristics of a small animal, having discernible feet, hindlimbs, tail, abdomen, and a tail.
Post-surgical evaluation of the foreign object revealed a foam-like dinosaur with a missing head that likely passed without obstruction.
Special Thanks to Metropolitan Animal Emergency and Specialty Center for the case follow-up and interesting case!
February's Case of the Month
Sonographer: Emily Evans, BVM&S
Investigation of anorexia after inconclusive barium study
Dr. Emily Evans
PATIENT INFORMATION:
Age: 10y 10m old
Gender: Male
Species: Canine
Breed: Pitbull
Weight: 62lbs
HISTORY:
Patient presented for several days of inappetence. Vomited once a week before examination and since has been eating very little and not defecating much. Routine lab work was all normal. Barium study showed dilation of duodenum that was consistent in multiple views with otherwise normal passage of ingesta.
SIGNIFICANT ULTRASOUND FINDINGS:
The stomach contained a mild-moderate amount of non-shadowing ingesta with mildly increased wall thickness. (5.1mm). The pylorus appeared free obstruction. There was a mild amount of digest in the duodenum but no significant distention or focal lesions. The jejunum became severely plicated and corrugated with increased wall thickness(up to 6.6mm) and irregular wall layering detail. The plicated area was traced to a severely hyperechoic thin linear structure creating a strong acoustic shadow(foreign material). Intestine around the structure was bunched and folded.
A mild amount of anechoic free fluid was seen throughout the abdomen. Mesentery around the plicated loops and the loop containing the foreign material was severely hyperechoic.
The prostate was found to be moderately-severe enlarged with hyperechoic coarse echogenicity and multifocal anechoic small cysts. No mineralization or focal lesions were noted.
The left testicle was atrophied and contained three hypoechoic nodules(0.9x0.5cm, 1.2x0.8cm, 0.5x0.4cm). The right testicle was a normal size, shape and echogenicity with no focal lesions. (Testicular size - Lt/Rt: 2.7x1.0/4.1x1.9cm)
The medial iliac lymph nodes were mildly plump and both had a few severely hypoechoic rounded nodules in the parenchyma
Multiple mesenteric lymph nodes are mildly enlarged with rounded shape having homogeneous hypoechoic echogenicity.
SONOGRAPHIC ANALYSIS:
Ultrasound findings were suggestive of a partially obstructive intestinal foreign body which was linear in appearance with no obvious anchoring. Free fluid, irregular folding and hyperechoic mesentery created concern for possible perforation(s) and/or adhesions.
Incidentally, significant left testicular atrophy and nodules were noted with concern for possible metastatic lesions in local lymph nodes. Associated benign prostatic hyperplasia was also identified.
Exploratory laparotomy and neuter(with biopsies of the left testicle) were recommended.
CASE OUTCOME:
Patient was taken to surgery for neuter and exploratory laparotomy. An affected loop of intestine had adhered to the dorsal body wall, the adhesions were broken down, intestinal perforations repaired and a corndog stick was removed with a single enterotomy site.
The patient has recovered from surgery and continues to do well at home. Biopsy of the testicle was declined. Recheck ultrasound is recommended in 60-90 days to assess prostate and lymph nodes.
Intestine/Foreign Body - Severely corrugated jejunum(first image) and thin severely hyperechoic linear structure causing dark acoustic shadow(second image).
Testicles: The atrophied left testicle has a coarse echotexture with lack of normal architecture and three hypoechoic well defined nodules.(Image 3) Right testicle for comparison. (Image 4)
Image 5 - Corndog stick removed via enterotomy. (Photo courtesy of Dr. Scott)
Special thanks to Dr. Taylor Scott at Locke A. Taylor, DVM Veterinary Hospital for the interesting case and follow-up!
January's Case of the Month
Sonographer: Shadawn Salmond-Jimenez, DVM
Sonographic Findings of Cor Triatriatum Dexter (CTD) in a Canine Puppy.
Dr. Shadawn Salmond-Jimenez
Patient Information:
Age: 2 months
Gender: Female Intact
Species: Canine
Breed: Labrador Retriever
History
Patient presented from another hospital where hepatomegaly was diagnosed on exam. A Grade II/VI murmur was ausculted on presentation. Patient was eating and drinking well with no clinical signs. Radiographs performed showed abdominal effusion (more than expected for the age). Thoracic radiographs showed dilation of the caudal vena cava, but otherwise normal thorax. An echocardiogram was requested and performed.
Echocardiogram Findings
A circular cystic structure is identified in the region of the left/right atrium. There is a trace of flow across the interatrial septum that is seen from several angles which likely represents flow through a patent foramen ovale.
Interpretation
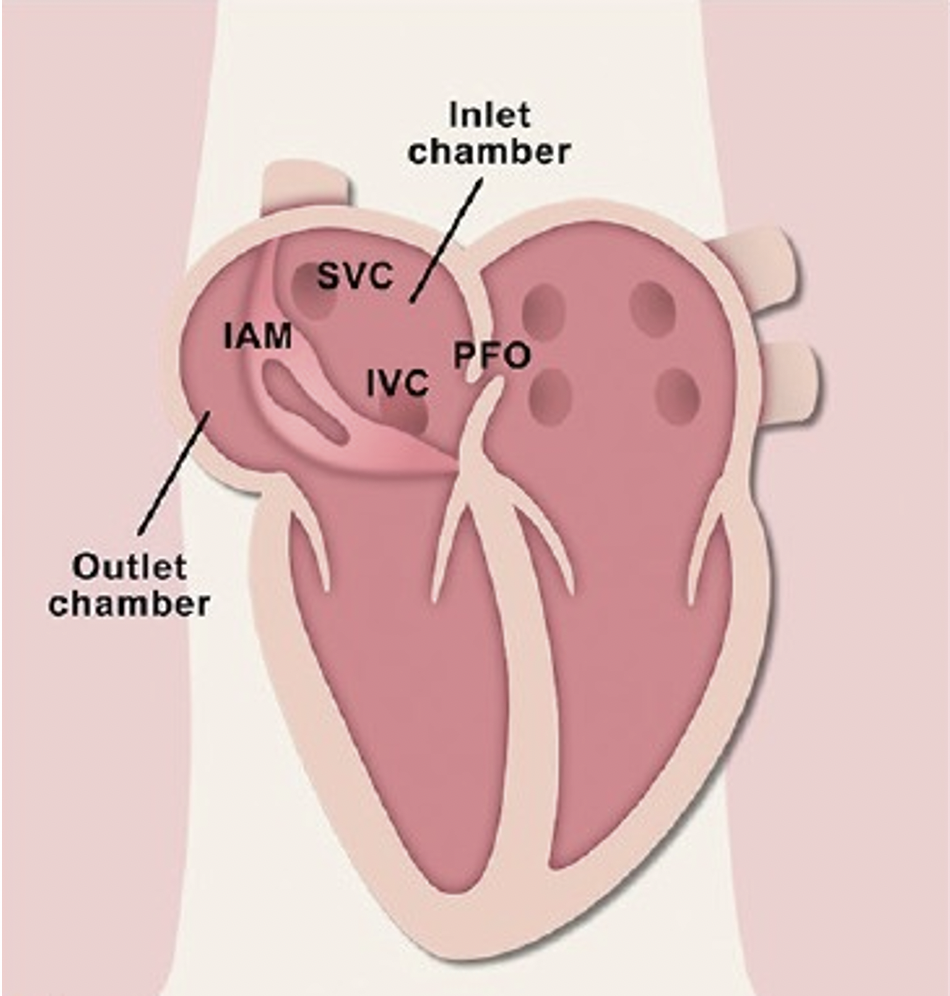
The cystic structure is likely a cor triatriatum dexter (CTD) which is a congenital defect where the right atrium is divided into a lower pressure cranial chamber that communicates with the tricuspid valve and higher pressure caudal chamber which may be the cause of the right to left flow through the PFO (Persistent Foramen Ovale).
Monitoring and Therapeutic Recommendations
The CTD may be an incidental finding but if signs of right-sided failure develop – ascites, treatment may be needed. Treatment involves balloon dilatation of the membrane and in rare cases stent implantation. Follow up is recommended.
Case Outcome
Surgical options pending clinical symptoms have been discussed. Patient remains asymptomatic.
Brief Summary of Cor Triatriatum Dexter
Cor Triatriatum Dexter (CTD) has been infrequently reported in dogs and the overall prevalence is low [1]. With this cardiac anomaly, the embryonic right valve of the sinus venosus fails to regress, resulting in partitioning of the right atrium (RA) into two distinct chambers and effectively creating a triatrial heart [2].
Given the varying extent of regression failure seen in different cases, the venous return from the abdomen to the RA can be impeded to varying degrees. This may result in clinical signs suggestive of caudal right-sided congestive heart failure (CHF) or a Budd-Chiari-like syndrome [3].
CTD can present with a variety of concurrent cardiac anomalies including persistent foramen ovale (PFO) (a hole between the left and right atria (upper chambers) of the heart).
For a positive long-term outcome balloon dilatation [5, 8, 19, 20], including cutting balloon techniques [20] or surgical correction under inflow occlusion or extracorporal circulation [2, 4, 10, 21, 22] have been reported as the treatment of choice.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5210289/
Cor triatriatum dextrum (Human Heart Illustration). IAM: Intra-atrial membrane partitioning the inlet and outlet chamber (Right Atrium), IVC: Inferior vena cava orifice, PFO: Patent foramen ovale, PV: Pulmonary vein orifice, SVC: Superior vena cava (Annals of Cardiac Anesthesia)
Above: Echocardiogram demonstrating a right long axis view of patient. A Large rounded thick walled structure (cystic structure) (blue arrow and blue asterisk) at the cavoatrial junction is seen between both normal atria (right atrium shown by yellow arrow and left atrium shown by pink arrow)
Below: Normal echocardiogram demonstrating a long axis view with normal left atrium (pink arrow) and right atrium (yellow arrow)
Above: Apical four-chamber view of the patient’s heart showing the cystic structure characteristic of cor triatriatum dexter (blue arrow) in the region of the right atrium (yellow arrow) and left atrium (pink arrow).
Below: Apical four-chamber view showing normal right atrium (yellow arrow) and left atrium (pink arrow).
A special thanks to DVM STAT Consulting for the echocardiogram interpretation and consultation and the staff at Prince Georges Animal Hospital for this interesting case.
November's Case of the Month
Sonographer: Kara Woody, DVM
Severe Gastric Ulceration in a Mixed Breed
Dr. Kara Woody
Patient Information:
Age: 8 years
Gender: Neutered Male
Breed: Mixed Breed
Species: Canine
History:
Patient presented with a history of vomiting and anorexia. “Coffee ground” vomitus and melena was noted by the owner. The patient had a fever and abdominal pain upon exam. No history of NSAID usage or other systemic illness.
Initial Diagnostics:
Prior to ultrasound, the patient had undergone a barium series in which barium transit was greatly prolonged. Foreign body was not suspected by the radiologist. Ultrasound was recommended for further evaluation.
Ultrasonographic Findings:
The stomach contains a small amount of fluid and gas/barium with moderately thickened walls up to 8.4mm and loss of normal layering distinction. There is multi-focal gas "capping" noted in the gastric mucosa. The tissue surrounding the caudal border of the stomach is moderately hyperechoic. The pylorus is free of obstruction.
Abdominal Ultrasound Interpretation:
Stomach - the findings are moderate - DDx: active gastritis vs. gastric ulceration with secondary granulation and thickening/edema vs. primary neoplasia vs. infiltrative neoplasia (lymphosarcoma, mast cell tumor, etc)
Recheck Exam:
Gastric ulceration was highly suspected based on history and ultrasound findings. The patient continued to decline despite aggressive treatment for ulceration. Additionally, extensive investigation was performed to identify an underlying cause of ulceration. A recheck ultrasound was recommended.
Ultrasonographic Findings:
The stomach contains a small amount of gas with a focally thickened wall in the fundus (up to 11.0mm; previously up to 8.4mm) and loss of normal layering distinction. There is multi-focal gas "capping" noted in the gastric mucosa (2.3mm width). The tissue surrounding the stomach is moderately hyperechoic. The rest of the stomach wall is normal thickness and layering. The pylorus is visualized and free from obstructions.
Abdominal Ultrasound Interpretation:
Stomach - the findings are moderate and PROGRESSED - DDx: active gastritis vs. gastric ulceration with secondary granulation and thickening/edema vs. primary neoplasia vs. infiltrative neoplasia (lymphosarcoma, mast cell tumor, etc)
Case Conclusion:
Unfortunately, no underlying cause for ulceration was identified. Patient condition continued to decline so humane euthanasia was elected. A necropsy was performed which revealed extensive mucosal ulceration of the gastric wall. The rest of the gastrointestinal tract and abdomen was within normal limits. Histopathology was not performed.
Discussion:
Gastric ulceration occurs when gastric acid production is increased or if the mucosal surface is compromised. Common causes include: liver disease, renal disease, Addison’s Disease, inflammatory bowel disease, and non-steroid inflammatory administration. Neoplastic causes include gastrinomas or mast cell tumors. Typically patients present with a history of vomiting, anorexia +/-hematemesis and/or melena. Fever, abdominal pain, diarrhea and lethargy also commonly occur. Treatments include H2 receptor antagonists, proton pump inhibitors, and prostaglandin E analogs and sucralfate. It is important to identify and treat the underlying cause if possible.
Focal severe thickness of fundic wall with loss of normal layering distinction.
Recheck @3 weeks -The wall remains severely thickened with loss of layering in the same location as previous.
Punctate hyperechoic foci (outlined by cursor) consistent with ulceration present within the gastric mucosa.
Thank you to Hilton Animal Hospital for collaborating with us on this interesting case.