March’s Case of the Month - 2024
Sonographer: Kara Woody DVM
Investigating Hypercalcemia in a Geriatric Canine
Patient Information:
Age: 13 years
Gender: Neutered Male
Breed: Maltese
Species: Canine
History:
Patient presented for lethargy and hyporexia. Elevated total calcium was present on laboratory work and confirmed with an ionized calcium. Additionally, renal values were normal. Abdominal ultrasound was recommended with top differential being neoplasia as cause of hypercalcemia.
Abdominal Ultrasonographic Findings and additional recommended diagnostics:
Abdominal ultrasound did not reveal an obvious cause of hypercalcemia. Mild chronic renal changes were present with mild diverticular mineralization (common in hypercalcemia) and mild adrenomegaly was present which was likely attributable to stress response. Given this, a cervical ultrasound was recommended to evaluate for any abnormalities in the parathyroids. Additionally, a PTH and PTHrp level was recommended as well as a rectal exam and 3 view thoracic radiographs.
Left Thyroid gland in sagittal with suspected enlarged parathyroid in the cranial gland.
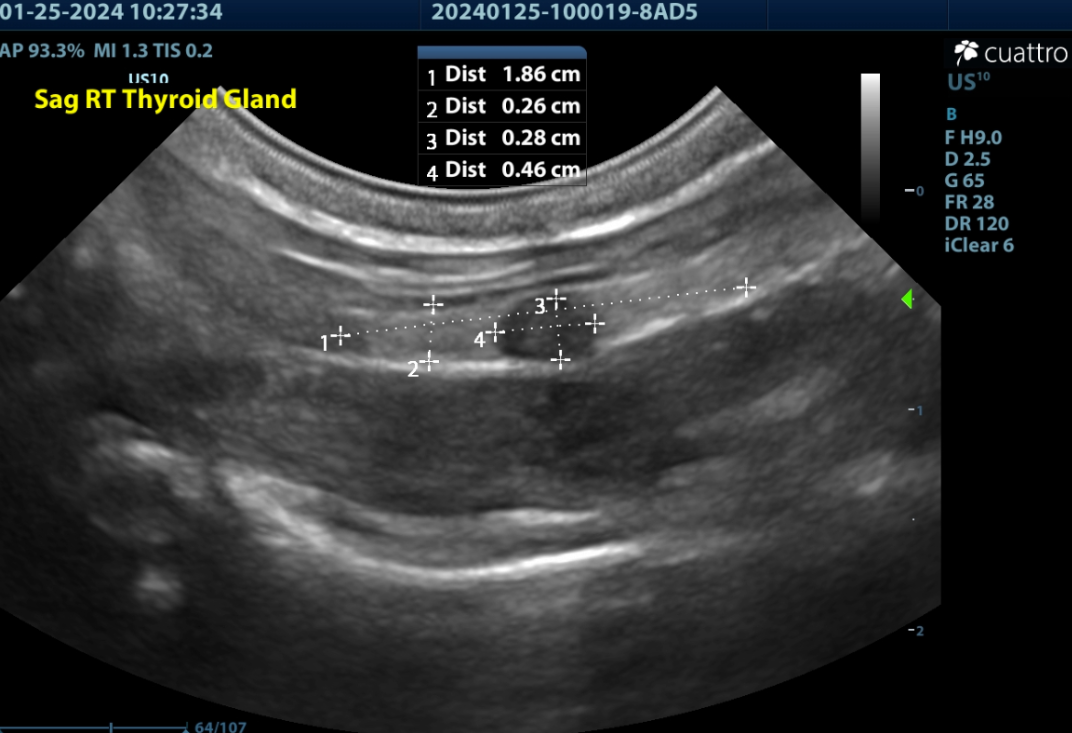
Right Thyroid gland in sagittal with suspected enlarged parathyroid in the mid gland; however, histopathology was consistent with Thyroid C-cell hyperplasia.
Right thyroid gland in transverse with color flow doppler showing the carotid and jugular vessels which are lateral to the thyroid gland. Note how the nodule mildly deforms the normal contour of the thyroid gland.
Left Thyroid Gland in transverse with a rounded hypoechoic nodule consistent with prominent parathyroid gland. Thyroid is located between the heavily shadowing trachea and the partially shadowing esophagus on the left side.
Left Thyroid gland in sagittal with suspected enlarged parathyroid in the cranial gland.
Right Thyroid gland in sagittal with suspected enlarged parathyroid in the mid gland; however, histopathology was consistent with Thyroid C-cell hyperplasia.
Right thyroid gland in transverse with color flow doppler showing the carotid and jugular vessels which are lateral to the thyroid gland. Note how the nodule mildly deforms the normal contour of the thyroid gland.
Left Thyroid Gland in transverse with a rounded hypoechoic nodule consistent with prominent parathyroid gland. Thyroid is located between the heavily shadowing trachea and the partially shadowing esophagus on the left side.
Cervical Ultrasound findings:
The thyroid glands are normal size, shape, and echogenicity. (Lt/Rt WXL=0.3x2.1cm/0.3x1.9cm)
Normal Small Dog Thyroid Length 17-23mm
Normal Small Dog Thyroid Width 3-5mm
There is a prominent homogenous hypoechoic rounded nodule noted in the cranial left thyroid measuring 2.2x2.9mm.
There is a prominent partially contour deforming heterogenous hypoechoic rounded nodule in the mid right thyroid measuring 2.8x4.6mm. Punctate cystic lesions are noted.
Normal Parathyroid Size = 2-3mm
Parathyroid Neoplasia > 4mm (mean of 7mm)
Parathyroid Hyperplasia > 2mm < 4mm (range 3-6mm)
The salivary glands contained punctate hyperechoic foci. (consistent with high calcium levels)
All other visualized structures-lymph nodes, trachea and esophagus are WNL.
Ultrasound Interpretation:
Bilateral thyroid nodules-the findings are moderate-DDx: parathyroid enlargement (diffuse hyperplasia vs. adenoma vs. adenomatous hyperplasia vs. adenocarcinoma) vs thyroid nodule (hyperplasia vs neoplasia)
**parathyroid hyperplasia and neoplasia can overlap in size and cannot be differentiated with ultrasound alone (both look the same sonographically) but requires histopathology to definitively diagnose. Thyroid nodules can also mimic parathyroid gland appearance and also require histopathology for definitive diagnosis.
Recommendations:
A surgical consult was recommended to remove both noted nodules if deemed appropriate at the time of surgery.
Surgical outcome:
The surgery was performed by a board certified traveling surgeon. An enlarged partially cystic nodule was found on the right thyroid. Additionally, the nodule on the left thyroid appeared to be an enlarged abnormal parathyroid gland and therefore was also removed. Both were submitted for biopsy and histopathology.
Histopathology Results:
Tissue submitted as parathyroid gland:
Right: Thyroid C-cell hyperplasia
Left: Parathyroid (chief cell) adenoma
Both were completely excised.
Discussion:
Differentials for hypercalcemia include, neoplasia (lymphosarcoma, apocrine gland adenocarcinoma of anal sac, as well as other carcinomas and select tumors), hypoadrenocorticism, renal failure, nutritional, Vitamin D toxicosis, granulomatous disease and primary hyperparathyroidism (parathyroid adenoma, hyperplasia or adenocarcinoma).
Ultrasonography is a reliable tool for identifying primary parathyroid disease. It has been found to be 90-95% accurate in identifying parathyroid adenomas. The most common presentation is a solitary parathyroid mass (typically adenoma); however, more than one adenoma, adenocarcinoma or hyperplasia can also occur and any abnormal appearing gland should be removed and biopsied at the time of surgery provided at least one functional parathyroid is left to maintain calcium homeostasis. Parathyroid glands and thyroid nodules can appear similar on ultrasound which is why surgical evaluation and biopsy is necessary for definitive diagnosis. Furthermore, it is important to always interpret ultrasound findings in light of laboratory findings. Specifically, PTH, PTHrp, and ionized calcium, BUN/Creatinine/phosphorus and urinalysis are recommended. Hyperplastic glands from secondary hyperparathyroidism (eg renal failure or nutritional) can mimic the appearance of primary hyperparathyroidism. If all 4 parathyroid glands are enlarged, particular care should be taken to ensure that primary hyperparathyroidism is the cause rather than secondary hyperparathyroidism.
Reference: Felman, EC and Nelson RW: Canine and feline endocrinology and reproduction-3rd ed. Philadelphia, WB Saunders, 2004. Pg 689-702.
This case illustrates the importance of identifying and removing any abnormal nodules within the thyroid glands in the face of hypercalcemia (after confirming suspicion of primary hyperparathyroidism as discussed above) and submitting any abnormal tissue for histopathology. Thyroid nodules and parathyroid glands can appear similar on ultrasound as well as grossly during surgery. In this case, the larger nodule was actually not an enlarged parathyroid gland, but a C-cell thyroid hyperplasia due to increased production of calcitonin due to elevated calcium levels. The actual parathyroid adenoma was located on the left thyroid. If only the larger nodule had been removed, then a cure would not have been obtained for this patient.
Case Outcome:
The patient recovered uneventfully from surgery. Initially calcium levels were low, which is common due to the atrophy of remaining parathyroid glands. The patient is currently receiving calcium carbonate and levels have normalized and the patient continues to do well.
Sonographer:
Kara Woody, DVM
Special thanks to Dr. Sebastian Gordon, DVM, DACVS (SA) at Lazar Veterinary Surgery and Banfield Stafford for collaboration on this interesting case!
February's Case of the Month- 2024
Sonographer: Anne Desrochers, DACVIM
Liver Shunt in a Dog
Patient Information:
Age: 11 weeks old
Species: Canine
Breed: Golden Retriever
Gender: Female
History:
The patient presented for ataxia and anorexia following a change in diet. Bloodwork revealed an elevated ALT (312U/L) and ammonia level, low albumin (2.0g/dL) and mild anemia (27.5%). Pre-prandial bile acids level was high at 106.4umol/L and post 149.2 umol/L.
Ultrasound Findings:
The liver was reduced in size but had a normal shape and echogenicity. In the right lateral liver lobe was a large tortuous aberrant vessel originating from a branch of the portal vein making a hairpin turn toward the caudal vena cava. The abnormal vessel measured up to 17.8mm in width and displayed turbulent blood pattern on color flow Doppler echocardiography. A right divisional intrahepatic portosystemic shunt was suspected.
Image 1. Sagittal plane of the right liver showing an intrahepatic connection of the portal vein branch (PV) with an anomalous dilated hepatic vessel (HV) looping towards the caudal vena cave (CVC).
Images 2. Sagittal plane color flow Doppler image showing turbulent blood flow within the shunt vessel indicated by the mosaic pattern of colors.
Surgical Consultation:
Treatment options included conservative medical management, surgical procedure, and interventional radiology. The decision was made to continue medical therapy (lactulose, antimicrobials, proton pump inhibitor, low protein diet and anticonvulsants as needed) and return when the patient had further grown for additional assessment. Over the next few months, the patient exhibited signs of stunted growth and episodes of seizure activity following dietary indiscretions. At the age of 8 months old, a CT scan with an angiogram contrast study was performed revealing a right divisional intra-hepatic shunt connecting a branch of the portal vein to the caudal vena cava. Percutaneous transjugular coil embolization for intrahepatic shunt attenuation procedure was carried out. Using fluoroscopy, a stent was placed in the vena cava via the jugular vein then embolization coils were placed in the shunt to occlude blood flow. Post-operative complications included transient gastrointestinal bleeding and signs of hepatic encephalopathy which were successfully managed.
Outcome:
Improvement in the hepatic function and mitigation of clinical signs were noticed overtime and shunt medications were tapered down. Additional coils placement has not been needed.
Special thanks to Dr. Grasso atAnimal Medical Center of Loudoun and Dr. Ganjei at VRA for their help with this case.
January's Case of the Month-2024
Sonographer: Danny Laderberg, DVM
A Twist of Events
Patient Information:
Age: ~4 years
Gender: Spayed Female
Species: Canine
Breed: English Bulldog
History:
Patient presented for lethargy, inappetence, and hematuria of a few days duration. Patient was pale upon presentation with firm organomegaly of the cranial abdomen on palpation. CBC showed anemia with a leukocytosis and hypoalbuminemia. Radiographs showed severe organomegaly cranial abdomen. A slide autoagglutination test was run and appeared positive. Patient was started on prednisone 30 mg SID and Clavamox 250 mg BID. Urinalysis show a possible infection as well.
Ultrasound Findings:
Liver: Mildly decreased in size, normal shape and echogenicity. No focal lesions are appreciated. The gall bladder is moderately distended with normal anechoic and hyperechoic unorganized dependent bile that is not resulting in obstruction. No common bile duct dilation is seen.
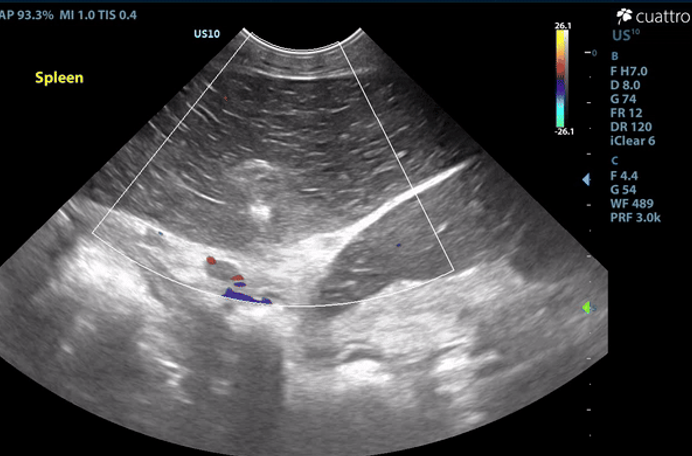
Spleen: The spleen measures 2.9 cm in depth and rounded in shape. There is diffuse hypoechoic echogenicity with hyperechoic linear striations creating a lacy echotexture. There is no appreciable blood flow noted throughout the splenic parenchyma with color flow doppler. The mesentery surrounding the spleen is moderately hyperechoic.
Image 1: Absent color flow doppler signal throughout the splenic parenchyma and vasculature. The spleen is diffusely hypoechoic with hypechoic linear striations producing a lacy echotexture.
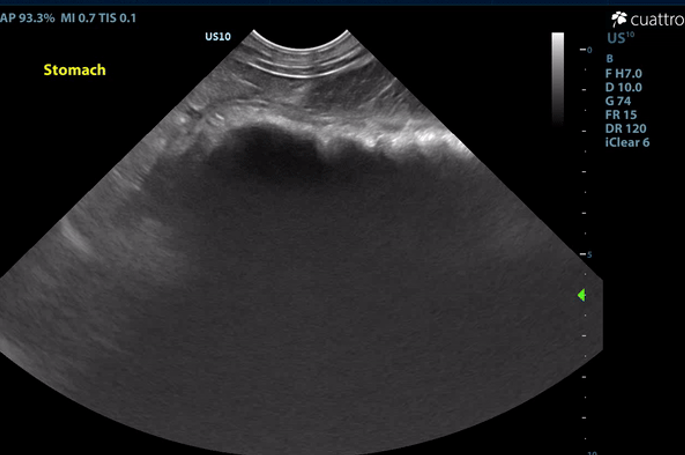
Intestinal Tract: The stomach contains a moderate amount of amorphous ingesta as well as amorphous,hyperechoic material associated with a strong anechoic shadow measuring ~7.8 cm in length. The stomach has normal visible wall thickness and layering. The pylorus is free of obstruction. Most loops of small intestine visualized have increased wall thickness measuring up to 6.0 mm with disproportionately large mucosal layers having hyperechoic radiating striations consistent with lymphangiectasia as well as echogenic stippling throughout. The bowel has increased overall motility and liquid contents.
No obstruction or masses seen. The colon has normal wall thickness and layering throughout.
Maximum thickness measurements: Stomach- 4.7mm; Duodenum- 2.8mm; Jejunum-6.0mm; Colon- 1.1 mm
Image 2: Hyperechoic material within the stomach creating a strong anechoic shadow.
Image 3: Linear striations diffusely throughout the mucosal layer of the jejunum consistent with dilated lacteals.
Serosal Surfaces: A mild amount of anechoic free fluid was noted throughout the abdomen. There is moderately hyperechoic mesenteric echogenicity. No focal lesions noted.
Abdominal Ultrasound Interpretation:
Spleen - the findings are severe - DDX: splenic torsion vs. infarct vs. infiltrative neoplasia vs open.
Intestines - the findings are moderate - DDx: protein-losing enteropathy (lymphangiectasia), lymphosarcoma, severe inflammatory bowel disease, histoplasmosis, lipogranulomatous lymphangitis). Rule-out protein-losing nephropathy (nephrotic syndrome) as source of protein loss.
Causes of Protein-Losing-Enteropathy (PLE)
A. Diseases affecting intestinal lymphatic drainage
Primary lymphangiectasia
Congenital or idiopathic acquired
Breed predisposition (including Yorkshire Terrier, Soft-coated Wheaten Terrier, Basenji, Norwegian Lundehund, and Chinese Shar-pei)
Secondary lymphangiectasia
IBD
Heterobilharzia americana
Neoplasia
Congestion secondary to right-sided heart failure or portal hypertension
B. Acute or chronic inflammatory diseases that result in increased mucosal permeability to protein
Inflammatory bowel disease (eosinophilic or lymphoplasmacytic enteritis)
Granulomatous enteritis (histoplasmosis, Pythiosis)
Intestinal neoplasia, (lymphoma, carcinoma)
Immunoproliferative enteropathy of Basenjis
Parasitic enteritis in young animals
Villous atrophy, gluten enteropathy, certain viral and bacterial enteritides
Chronic obstruction or intussusception
C. Gastrointestinal Blood Loss
Bleeding tumors
Ulceration/erosion
Intestinal parasites (Hookworms)
Gastric Foreign Body - the findings are moderate and suggestive of an intraluminal gastric foreign body vs. recently ingested bone/chew/etc. vs. open
Microhepatica (decreased hepatic mass) The findings are mild - DDX: Chronic hepatic disease with progressive loss of hepatocytes (cirrhosis or pre-cirrhosis) Decreased portal blood flow with hepatocellular atrophy
Congenital portosystemic shunt
Intrahepatic portal vein hypoplasia (presumptive diagnosis - biopsy confirmation is necessary)
Chronic portal vein thrombosis
Hypovolemia
Hypoadrenocorticism
Ascites - this finding is mild - DDx: transudate vs. hemorrhagic vs. exudate
Mesentery - the findings are moderate - DDx: peritonitis - inflammation vs. paraneoplastic reaction vs. infectious vs. fibrosis vs. other.
Recommendations:
The splenic appearance and lack of color flow doppler signal is consistent with a splenic torsion or infarct. Exploratory laparotomy is recommended for splenectomy and histopathology.
The ingesta within the stomach is associated with strong anechoic shadow which can be consistent with foreign material. Exploratory laparotomy is recommended for further evaluation of the intestinal tract and gastrotomy if indicated. The changes to the small intestinal tract are consistent with dilated lacteals, a common finding seen in dogs with a protein-losing enteropathy (PLE). Given the reported hypoalbuminemia (1.5 g/dL), PLE would be a primary differential in this patient. If surgery elected, GI biopsies are recommended to better define the nature of the disease present. Consider submitting a Texas A&M GI panel and switching to a strict novel protein diet if not already done.
The cause of Rogue's anemia (HCT 15%) is not definitively identified in this study. While anemia is a common comorbidity associated with splenic torsion, further investigation is necessary to assess the true etiology, especially in light a positive slide agglutination test. A CBC with pathology review is recommended to assess for regenerative changes, red blood cell morphologies, red blood cell pathogens, etc. A tick PCR panel should also be considered to assess for inciting causes of immune mediated anemia.
Abdominocentesis of the ascites noted is recommended for fluid analysis/cytology to better assess the nature of the fluid present and to help rule out blood loss as a cause of anemia. While GI protein loss is the most likely differential, investigation into alternative etiologies is recommended. Consider liver function test and urinalysis with UPC after resolution of reported urinary tract infection. Liver biopsies should also be considered if surgery is elected.
Given the degree of anemia, a red blood cell transfusion is recommended prior to surgery. A clotting profile would also be recommended prior. If transfusion is elected, blood should be collected for pathology review prior to transfusion. Consider other diagnostics/therapeutics as clinical signs dictate.
Outcome/Further Testing:
Unfortunately, the owner elected for humane euthanasia due to financial constraints.
Necropsy: Post-mortem abdominal exploratory confirmed a splenic torsion, serous ascites, as well as cloth material within the stomach.
Image 4: Gastric foreign material.
Image 5: Splenic torsion.
Image 6: Right lateral radiograph.
Image 7: VD radiograph.
Discussion:
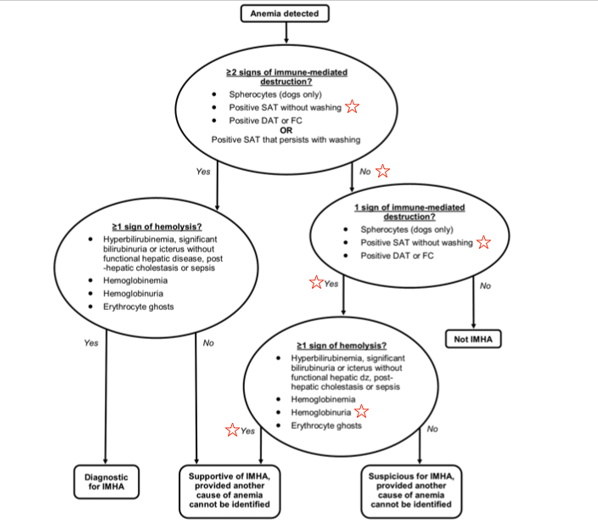
Multiple pathologies were discovered in this patient, most notably a gastric foreign body, primary splenic torsion (PST), and dilated lacteals consistent with protein-losing enteropathy. Notable clinical pathologies established prior to the ultrasound study included a marked anemia (15.9%), moderate leukocytosis (20.2 K), and severe hypoalbuminemia (1.5 g/dL). A positive saline agglutination test (SAT) was also noted. Bacteriuria (rods and cocci), hemoglobinuria, and mild pyuria (3 WBC/hpf) were also noted via SediVue Analyzer, but manual cytology was not reported. The interconnectivity of these pathologies will be discussed further here.
There are three broad categorical causes of anemia5:
1) Decreased production (anemia of chronic disease such as erythropoietin-related conditions or iron-deficiencies and bone marrow conditions)
2) Loss (hemorrhage)
3) Destruction (hemolysis, oxidative injury, parasitic, toxicity, etc.)
Further investigation would be necessary to fully elucidate the true etiology/etiologies, however, reasonable assumptions may be made to better understand the anemia. The initial concern for this patient’s anemia was presumed to be an immune-mediated disease (IMHA) due to the degree of anemia, positive saline agglutination test (SAT), and presence of hemoglobinuria. The mechanism of hemoglobinuria in PST dogs is suspected to be secondary to intravascular or intrasplenic (extravascular) hemolysis.2 Based on the ACVIM consensus statement on the diagnosis of immune-mediated hemolytic anemia, this patient would be classified as ‘supportive of IMHA, provided another cause of anemia cannot be identified.’1 [See Figure 1] However, a positive SAT can be a result of RBC rouleaux formation and rouleaux formation can be promoted in hypoalbuminemic patients.4 Further dilution and cytology would be necessary to differentiate between true agglutination versus rouleaux formation in light of a positive SAT. A CBC with pathology review would also be beneficial in this case to assess for regenerative changes, red blood cell morphologies, red blood cell pathogens, etc. to further strengthen the argument for a hemolytic cause of anemia. Given the exhaustive list of reported inciting causes of IMHA, this patient, coincidentally or not, has multiple listed morbidities associated with triggering IMHA (i.e. inflammatory disease, necrosis, urinary tract infection, etc.).
Figure 1: IMHA diagnostic algorithm as presented in the ACVIM consensus statement1
While an argument can be made for immune-mediated disease, when incorporating the physical exam findings into the assessment of the patient’s anemia, decreased production/chronic anemia could be considered the most likely, or most substantial, etiology. On physical exam, the patient was found to be alert and responsive, pale, cachectic with a BCS of 2/9 and MCS of 1/5, eupneic, with a normal heart rate of ~100 BPM, all suggesting chronic disease. In the face of an acute onset marked anemia (as commonly seen with IMHA), tachypnea, tachycardia, and associated mentation changes/weakness would be expected. An elevated bilirubin would also be suspected, especially given the degree of anemia. In the same light, RBC loss/hemorrhage would also be considered less likely (and largely ruled out in this case as the ascites on necropsy was grossly serous fluid and no evidence of hematochezia, melena, and only mild true hematuria [7 RBC/hpf]). Ultimately, the true cause of anemia is likely multifactorial in this patient.
Primary splenic torsion (PST) is rare and the etiology is poorly understood. Acute and chronic PST have been reported, and English Bulldogs are an over-represented breed, accounting for up to 11.8% of cases.3 Clinical signs associated with acute PST include abdominal pain and distention, vomiting, depression, and anorexia. Chronic PST presents with varying clinical signs including anorexia, weight loss, intermittent vomiting, abdominal distention, PU-PD, hemoglobinuria, and abdominal pain.3 It is difficult to determine the chronicity of the PST in this case. The owner reported a few day history of hyporexia, lethargy, and hematuria. Given the poor body and muscle condition, morbidities predating a few days are almost certain, however a chronic gastric foreign body and enteropathy (presumed PLE) may have predated and, in some theoretical manner, aided in a more acute onset PST. Given the over-representation of the breed, a genetic predisposition such as absent or weak gastrosplenic and/or phrenicosplenic ligaments may be a contributing factor.
Lack of reported historical vomiting and diarrhea makes assumptions of a chronic foreign body and PLE difficult. While diarrhea is the most commonly reported clinical sign associated with PLE, some studies show upwards of 33% of cases have no reported diarrhea.6 The marked hypoalbuminemia, along with the prominent mucosal changes noted, makes a PLE the most likely diagnosis for the cause of this patients hypoalbuminemia. GI biopsies would be necessary for a definitive diagnosis. Notable alternative etiologies such liver dysfunction, protein-losing nephropathies (PLN), malnutrition, and parasitism could also be considered. While the liver appeared subjectively decreased in size, aside from hypoalbuminemia, there were no direct or indirect hepatic markers on baseline labwork to suggest liver dysfunction (normal liver enzymes, cholesterol, bilirubin, globulins, and elevated glucose). Ultimately, liver function tests +/- biopsies would be necessary to rule out liver dysfunction as a cause of the hypoalbuminemia. A urine protein:creatinine ratio would also be indicated to assess for potential protein-losing nephropathies (PLN) following the resolution of the reported urinary tract infection. Fecal analysis and empirical deworming would also be indicated. All things considered, given the degree of weight loss, hypoalbuminemia, and mucosal changes, a chronic PLE would be the primary differential in this patient. Additionally, while uncommon to see both a diffuse enteropathy and gastric foreign material in the same patient, foreign body ingestion (pica) is not an uncommon manifestation of chronic GI disease in dogs.
Overall, this case presents an interesting constellation of clinical signs and pathologies that highlights the value and utility of ultrasound in veterinary practice.
References:
1. Garden OA, Kidd L, Mexas AM, Chang YM, Jeffery U, Blois SL, Fogle JE, MacNeill AL, Lubas G, Birkenheuer A, Buoncompagni S, Dandrieux JRS, Di Loria A, Fellman CL, Glanemann B, Goggs R, Granick JL, LeVine DN, Sharp CR, Smith-Carr S, Swann JW, Szladovits B. ACVIM consensus statement on the diagnosis of immune-mediated hemolytic anemia in dogs and cats. J Vet Intern Med. 2019 Mar;33(2):313-334. doi: 10.1111/jvim.15441. Epub 2019 Feb 26. PMID: 30806491; PMCID: PMC6430921.
2. Nelson, Richard W., and C. Guillermo Couto. “Chapter 86: Lymphadenopathy and Splenomegaly.” Small Animal Internal Medicine, Elsevier/Mosby, St. Louis, MO, 2014.
3. DeGroot W, Giuffrida MA, Rubin J, Runge JJ, Zide A, Mayhew PD, Culp WT, Mankin KT, Amsellem PM, Petrukovich B, Ringwood PB, Case JB, Singh A. Primary splenic torsion in dogs: 102 cases (1992-2014). J Am Vet Med Assoc. 2016 Mar 15;248(6):661-8. doi: 10.2460/javma.248.6.661. PMID: 26953920.
4. “Pattern Changes.” eClinpath, 18 Oct. 2016, eclinpath.com/hematology/morphologic-features/red-blood-cells/patterns/.
5. Thompson, Mark S. Small Animal Medical Differential Diagnosis (Third Edition). W B Saunders Company, 2018.
6. Simmerson SM, Armstrong PJ, Wünschmann A, Jessen CR, Crews LJ, Washabau RJ. Clinical features, intestinal histopathology, and outcome in protein-losing enteropathy in Yorkshire Terrier dogs. J Vet Intern Med. 2014 Mar-Apr;28(2):331-7. doi: 10.1111/jvim.12291. Epub 2014 Jan 27. PMID: 24467282; PMCID: PMC4857982.
December’s Case of the Month-2023
Sonographer: Meredith Adams, DVM
Feline Plasma Cell Tumor in Multiple Locations
Patient Information
Age: 12 years
Gender: Castrated Male
Breed: Domestic Medium Hair cat
Weight: 11 pounds
History
Presented for abdominal ultrasound to evaluate for underlying cause of anorexia, lethargy, weight loss and recent history of diarrhea. A firm grape sized nodule was also noted on the top of the patient’s head.
Abdominal ultrasound findings
Kidneys: Both kidneys have normal size (Lt/Rt = 3.5/3.6cm ) and normal shape with coarse mild to moderately hyperechoic renal cortices which are disproportionately large. There is mild loss of the corticomedullary junction distinction. No pyelectasia seen. There is a small (0.3x0.4cm) hypoechoic homogenous nodule in the left kidney.
Spleen: Mildly enlarged (1.3cm depth) with mildly rounded shape and normal echogenicity. No focal lesions appreciated.
Bladder: The bladder is moderately distended with anechoic urine and is of relatively normal contour and thickness. There is a small 0.3x0.2cm bladder wall nodule in the right mid-caudal bladder.
Gastrointestinal Tract
The stomach is empty and collapsed with normal rugal folds and layering.
Many loops of intestine are prominent and mildly to moderately thickened (Duodenum 3.1mm; Jejunum 2.6-3.1 mm (normal wall thickness ~2.2-2.5mm, > 2.8mm abnormal Norsworthy/Estep et. al. JAVMA, Vol 243, No. 10, November 15, 2013)). Some have abnormal layering with prominent disproportionate thickening of the muscularis layer.
The colon is mildly thickened (2.0mm) and has normal layering throughout.
Differentials Splenomegaly: the findings are mild DDx. neoplasia (mast cell, lymphoma, carcinoma, metastatic disease) vs. fungal (Histoplasmosis) vs. reactive lymphoid hyperplasia vs. splenitis vs. congestion vs. extramedullary hematopoiesis (EMH).
Intestines: the findings are mild DDx. inflammatory bowel disease/food intolerance vs. infiltrative neoplasia (small-cell lymphosarcoma vs. mast cell tumor) vs. parasitism (cestode) vs. dry FIP vs. fungal (histoplasmosis). Inflammatory bowel disease in cats can be chronic and long-standing but in many cases will transition into small-cell lymphosarcoma and it is not possible with ultrasound alone to determine in this case whether the disease is benign or infiltrative.
Inflammation of Large Intestine: the findings are mild DDx. Acute colitis/proctitis vs. Chronic colitis (Lymphocytic/plasmacytic colitis vs. Eosinophilic enterocolitis vs. Chronic ulcerative colitis) vs. IBS
Bladder Nodule: the findings are mild DDx. Tumors of the urinary bladder are uncommon in dogs and rare in cats. Transitional cell carcinoma (TCC) is the most common primary tumor of the urinary bladder in both species. Other differentials include squamous cell carcinoma, leiomyosarcoma, leiomyoma, and rhabdomyosarcoma or benign bladder polyp. The bladder may also be invaded by prostatic neoplasia or metastatic disease (e.g., hemangiosarcoma, lymphoma). Bacterial cystitis and urolithiasis are common differentials for the clinical signs seen, and a rare but important differential diagnosis for mass lesions is benign polyps of the urinary bladder.
Additional Diagnostics
Ultrasound guided fine needle aspirates of the spleen were obtained for cytology. A fine needle aspirate of the nodule on the head was also performed. Samples of both sites were submitted to Eastern Vet Path for analysis.
Cytology Microscopic Description
Nodule on top of head: The slides are lightly to highly cellular and consist of few to many red blood cells and a nucleated cell population predominated by individual round cells with very low numbers of neutrophils and small lymphocytes. These round cells have a moderate amount of basophilic cytoplasm, and occasional prominent perinuclear clear area, and eccentric, round two lobulated nuclei. The nuclei have a densely clumped chromatin pattern. Anisokaryosis is mild; bi nucleation is rarely noted. Occasional mitotic figures are present. See photo below.
Spleen: the slides are of low to high cellularity with few to several red blood cells. Large round cells that resemble those found in the nodule predominate. Few small lymphocytes, occasional neutrophils and rare macrophages are also present.
COMMENTS
For both locations, cytologic findings are consistent with a plasma cell tumor, 90-100% confidence. If not already performed, consider measuring globulin concentration ± SPE. Screening the liver and bone marrow may also be considered
Diagnosis
Nodule on top of head: Plasma cell tumor
Spleen: Plasma cell tumor
Discussion
Unexpectedly, both fine needle aspirates revealed the same disease, plasma cell tumor, suggesting metastatic disease and/or multiple myeloma.This patient was sedated, so splenomegaly could have been secondary to sedative medications. The nodule on the head had many other differentials as well. Aspiration of abnormal findings can often yield rewarding diagnostic results even when unexpected.
Outcome
Additional diagnostics to consider for this patient would include measuring globulin concentration ± serum protein electrophoresis. Screening the liver and bone marrow may also be considered. Referral for oncology consultation and a recheck sonogram to monitor the nodule in the kidney and in the bladder was also recommended. Unfortunately, this patient was humanely euthanized due to poor clinical condition and diagnosis of neoplasia
November's Case of the Month-2023
Sonographer: Emily Evans DVM
Lymphoma with Focal Renal Lesion
SIGNALMENT:
Age: 9y 6m
Gender: Female Spayed
Species:Feline
Breed:DSH
Weight: 6lb
HISTORY:
The patient presented for weight loss. Abdominal palpation revealed kidney shape irregularities and concern for an abdominal mass. An abdominal ultrasound was requested to better evaluate the palpation findings and look for causes of weight loss.
ULTRASOUND FINDINGS AND IMAGES:
Kidneys - Normal size(Lt/Rt: 3.9/ 4.0cm)with a normal to mildly elongated shaped having heterogeneous hypoechoic echotexture in the cortex and medulla. There is trace/mild hypoechoic subcapsular fluid present. There is a hypoechoic, mildly vascular, rounded, well defined capsule altering nodule protruding from the cranial pole of the right kidney.(1.1x1.0cm) No pyelectasia was noted.
Image 1: Right Kidney with cranial pole capsule altering hypoechoic nodule with trace subcapsular fluid.
Bladder - The bladder is moderately distended with mildly echogenic urine with amorphous suspended debris and is of relatively normal contour and thickness. No overt obstruction, uroliths, or neoplasia noted.
Small intestine - Many to most loops of intestine are prominent and mildly to severely thickened. Duodenum 3.1-3.7mm, Jejunum 2.7-4.5mm, Ileum 6.4mm (normal wall thickness ~2.2-2.5mm, > 2.8mm abnormal Norsworthy/Estep et. al. JAVMA, Vol 243, No. 10, November 15, 2013). Many have abnormal layering with prominent disproportionate thickening of the muscularis layer.
Lymph nodes - Multiple mesenteric lymph nodes are severely enlarged with rounded shape having homogenous hypoechoic echogenicity.(~3.5x2.3cm) The ICCJ lymph nodes are mildly hypoechoic and plump. (0.7cm)
Image 2: Enlarged hypoechoic heterogenous mesenteric lymph node with hyperechoic mesentery.
Serosal Surfaces There is a trace amount of free fluid in the abdomen. Mesentery throughout the abdomen is diffusely hyperechoic.
ABDOMINAL ULTRASOUND INTERPRETATION:
Lymph nodes - the findings are severe - DDx: infiltrative neoplasia (lymphoma vs. mast cell vs. other) vs. IBD vs. infection vs. reaction vs. metastatic neoplasia
Kidneys - the findings are mild-moderate - DDX:
Chronic nonspecific change- (chronic glomerulonephritis vs. amyloidosis), chronic interstitial nephritis, chronic nephritis
Acute renal failure/Nephritis (infectious, GN, toxic, etc.) vs. Acute-on-Chronic renal failure.
Lymphosarcoma
Pyelonephritis
Right Kidney Nodule - the findings are moderate -DDx: renal lymphosarcoma - may appear as diffuse disease or focal mass, primary renal carcinoma, primary renal TCC, renal malignant histiocytosis or mastocytosis, malignant osteosarcoma, hemangiosarcoma - metastatic VS. fungal infection (Cryptococcus or Aspergillosis)
Intestines - the findings are mild-severe - DDX: inflammatory bowel disease/food intolerance vs. infiltrative neoplasia (small-cell lymphosarcoma vs. mast cell tumor) vs. parasitism (cestode) vs. dry FIP vs. fungal (histoplasmosis).
Ascites- this finding is mild - DDx: transudate vs. hemorrhagic vs. exudate
Mesentery - the findings are mild-moderate - DDx: peritonitis - inflammation vs. paraneoplastic reaction vs. infectious vs. fibrosis vs. other.
Echogenic urine - Ddx: cellular vs. lipid vs. protein vs. amorphous debris
FURTHER TESTING:
Ultrasound guided free hand biopsies of the mesenteric lymph node and the kidney nodule were collected for cytology.
CYTOLOGIC DIAGNOSIS AND FINDINGS:
Kidney Nodule: High-grade granular lymphoma
Mesenteric lymph node: High-grade granular lymphoma
The diagnosis of high-grade lymphoma is definitive (100% confidence), for both locations. The granular morphology is consistent with lymphocytes of cytotoxic T cell or possibly NK cell origin.
MICROSCOPIC DESCRIPTION:
The slides from the two locations appear very similar, are moderately to highly cellular, and consist of few red blood cells and a nucleated cell population predominated by large immature lymphocytes, with few small lymphocytes, and occasional neutrophils. The large lymphocytes consist of a small amount of basophilic cytoplasm that occasionally contain few small pink manuals, a perinuclear clear area, and a large round nucleus with a finely-stippled chromatin pattern and 1-3 prominent nucleoli. Occasional mitotic figures are noted. The background consists of many lymphoglandular bodies and occasional free nuclei.
Image 3:Kidney: Numerous large immature lymphocytes
DISCUSSION:
Lymphoma is a commonly found neoplasia of feline patients. These patients may present with vague clinical signs such as weight loss and malaise. The incidence of renal involvement in feline lymphoma patients is estimated to be 3.6% to 30%. Multicentric lymphoma is suspected in this patient due to a focal renal lesion(rather than bilateral renal enlargement) and lymph node involvement with intestinal changes suggestive of lymphoma.
OUTCOME:
The referring veterinarian and patient owner are performing additional baseline diagnostics and discussing options for treatment.
REFERENCES:
Debruyn K, Haers H, Combes A, et al. Ultrasonography of the feline kidney: Technique, anatomy and changes associated with disease. Journal of Feline Medicine and Surgery. 2012; 14 (11): 794-803. doi: 10.1177/1098612X12464461
Valdés-Martínez A, Cianciolo R, Mai W. Association between renal hypoechoic subcapsular thickening and lymphosarcoma in cats. Vet Radiol Ultrasound. 2007 Jul-Aug;48(4):357-60. doi: 10.1111/j.1740-8261.2007.00256.x. PMID: 17691636.
The Curbside guide- Diagnosis & Treatment of Common Sonographically Detected Disease: Canine & Feline; Lindquist/ Frank/ Modler Lobetti, 2015, Sonopath LLC., pp. 181
Williams AG, Hohenhaus AE, Lamb KE. Incidence and treatment of feline renal lymphoma: 27 cases. J Feline Med Surg, 2021 Oct;23 (10):936-944. doi: 10.1177/1098612X20984363. Epub 2021 Jan 19. PMID: 33464143
Jeon J, Song D, Ro W, Kim H, Lee G, Cho J, Jeong W, Kim S, Sur J, Park H. Renal Lymphoma with Mesenteric Lymphomatosis in a Cat. J Vet Clin 2020;37:208-212. https://doi.org/10.17555/jvc.2020.08.37.4.208
Thank you Hope Animal Hospital and Eastern Vet Path for collaborating with us on this case !
October's Case of the Month - 2023
Sonographer: Mallory Repellin DVM
How Many Specialists Does It Take to Diagnose a Mass?
Patient information:
Age: 3 years
Gender: Female (suspected Spayed per rDVM)
Breed: Golden Retriever
Species: Canine
History:
Sandy was evaluated at her RDVM for weight loss, inappetance and urinary incontinence on 5/11/2023. Exam revealed a large palpable mass on right dorsocranial abdomen.
Ultrasonographic findings:
Kidneys: Only the left kidney was readily visible. Enlarged size (Lt = 9.4 cm) and normal shape with normal corticomedullary dimensions. Moderate pyelectasia visualized (7.5 mm).
The right kidney appears severely hydronephrotic with minimally discernible septum creating a kidney- reminiscent shape, measured approximately 12.9 cm.
There is a heterogenous, hyperechoic, peripherally vascular mass which appears to protrude into the area of the renal pelvis from the proximal ureter. Mass width exceeded the scope of the ultrasound probe (at least 9.4 cm), mass depth is at least 8.7 cm.
Intestines: There is a focally mildly thickened segment of small intestine (max thickness 5.0 mm) with no sign of infiltrative disease.
Abdominal ultrasound interpretation:
Right hydronephrosis- the findings are severe- secondary to ureteral obstruction
Right ureteral mass- the findings are severe- Ddx: carcinoma (TCC/UC, other), soft tissue sarcoma, less likely granuloma Left Kidney
Pyelectasia DDX:
a) IV fluid administration
b) Pyelonephritis and ureteritis
c) Increased diuresis caused by renal insufficiency or other condition
d) Toxin
e) Infectious (leptospira, etc)
f) Post-renal obstruction / Bladder distention
g) Diuresis
Images:
Image 1: Significant pyelectasia noted in the left renal pelvis.
Image 2: Hydrodronephrosis of the right kidney with soft tissue mass in the caudal pole suspected to be causing right ureter obstruction.
Image 3: Right caudolateral mass effect which extends beyond the scope of ultrasound probe, located between the abnormal right kidney and cranial aspect of the urinary bladder.
Recommendations:
Referral to a veterinary surgeon for further diagnostics (CT scan, chest and abdomen) and therapy is highly recommended.
Additional tests:
CT scan:
Variable but small volume fluid is noted in the peritoneal space
In the region of the right kidney there is a large fluid-filled structure identified with a more soft tissue rim, thought to represent the renal capsule. It has a tubular extension medially and slightly caudally, through to be the right ureter which cannot be followed to the urinary bladder. This is followed caudally towards an at least 11 cm x 8.5 cm, irregularly marginated, soft tissue attenuating and heterogeneously enhancing, mildly complex mass located in the caudal abdomen to the right of midline, questionably retroperitoneal in location.
Moderate left renal pelvic dilation also identified, tracing into a dilated left ureter which is mildly tortuous and also cannot be traced to the level of the urinary bladder due to the large mass-effect. This mass is also noted to be displacing the caudal vena cava and associated more caudal branches dorsally with at least compression although invasion cannot be entirely excluded, especially caudal to the level of the renal parenchyma.
The right renal vein is not specifically outlined. The aortic and additional sublumbar including the medial ilial lymph nodes bilaterally, are variably enlarged although somewhat summetrically.
Both adrenal glands are difficult to specifically distinguish although thought to be seen separate from this mass-like change and both at least mildly enlarged.
Conclusions: Large, more right-sided, complex soft tissue mass with regional peritoneal and retroperitoneal effusion. It is unclear as to whether this is a more caudally positioned right kidney mass (less likely) over a caudal retroperitoneal cavitary mass with chronic obstruction of the ureters, more severe on the right with resulting hydronephrosis and lack of renal parenchyma. More moderate to marked left pyelectasia to early hydronephrosis identified with chronic at least partial obstruction from this mass. Neoplasia is thought most likely and given the location hemangiosarcoma may be the primary differential over round cell neoplasia or carcinoma. Right ureteral origin mass not excluded although would be difficult to confirm with the size of this mass and expansile appearance. It is unclear as to whether guided FNA would provide additional information and biopsy may be indicated. Given the appearance surgical removal could be attempted although invasion into the caudal aspect of the caudal vena cava and involvement of the ureters cannot be specifically determined tomographically.
Photo: CT scanned image displaying the enormity of the mass prior used for surgical planning.
Surgery report:
Multiple firm, small, non-movable masses were present within the internal rectus sheath, within the abdominal cavity.
An extremely large, extensive, firm and complex mass was present in the right mid to caudal abdomen, extending past midline adjacent to the pelvic brin. Upon further evaluation, and wafter careful dissection of some of the surrounding omental adhesions to the mass, the mass was extremely complex and firm, with multiple organs adhered to or into the mass, including the mid to distal duodenunum, the descending colon, the right kidney, the right ureter, the uterine stump, the apex of the urinary bladder, the caudal vena cava, aorta, and femoral arteries.
The right kidney was markedly distended, soft, and fluid filled, resembling a large water balloon (it measured approximately 12 cm in length, and the mass was another 9-10 cm in length, 8 cm wide.
The segment of mid to distal duodenum, including the caudal duodenal flexure, were noted to be completely embedded within the mass and were visually blocking the ability to discern the dorsal margin of the mass.
Once the embedded duodenal segment "removed," the dorsal and medial margins of the mass could be visualized; the caudal vena cava and aorta were noted cranially to the mass, and then lost into the mass caudal to the left kidney. The mass appeared to have both a peritoneal and retroperitoneal component.
A partial cystectomy was performed as the apical aspect of the urinary bladder and the distal aspect of the uterine stump were completely embedded within the mass.
The distal aspect of the right ureter was noted to be entering into the urinary bladder, but the remaining proximal portion was completely embedded and lost into the mass. The mass also seemed to be firmly adhered to underlying epaxial musculature at the level of the mid ureter.
An additional extension of the mass was noted immediately dorsal to a segment of descending colon, which was deviated dorsally (due to the mass). The sacral lymph node could be visualized and was enlarged and firm.
Cytoreductive surgical removal of the most ventral aspect of the mass (the inside of the mass was caseous and gritty in appearance, with a brown to white exudate) was performed, and approximately 3/4 of the mass was removed.
Photo 1: The excised bulk portion of the right abdominal mass which includes the right kidney, small intestines, colon, ureters and indiscriminate mesentery.
Photo 2: The excised bulk portion of the right abdominal mass which includes the right kidney, small intestines, colon, ureters and indiscriminate mesentery (slightly different angle).
Histopathology report:
Pathological Findings, Diagnosis
Omental nodules: Severe, chronic, pyogranulomatous omentitis with suspected intralesional yeast or algae
Right retroperitoneal mass: Severe, chronic, pyogranulomatous retroperitonitis and nephritis with intralesional yeast or algae
Comments
Both the omental nodules and the retroperitoneal mass were caused by severe, chronic, pyogranulomatous inflammation, and the nodular inflammation often surrounded groups of suspected yeast or possibly algae (i.e. Prototheca). The inflammation and suspected organisms also infiltrated and disrupted much of the kidney in the retroperitoneal sample. Due to the negative staining of the suspected organisms, further differentiation could not be performed with routine staining.
Microscopic Description
Omental nodules (slide A) - Sections of omental fat are examined in which the fat is infiltrated by inflammatory nodules that are composed of coalescing dense groups of macrophages that surround and are mixed with large numbers of neutrophils. At the center of some nodular groups of inflammation were region of necrosis containing vague, negatively staining, round, possible fungal yeast or algal organisms that are 10 -30um in diameter. Mature, dense fibrosis dissects through and surrounds the regions of inflammation. Small numbers of lymphocytes and plasma cells are also throughout, and there are some regions of edema and hemorrhage.
Right retroperitoneal mass (slides B1 – B3) – The retroperitoneal fat and much of the kidney are infiltrated by severe, nodular pyogranulomatous inflammation with similar features to the inflammation described above in the omentum. At the center of many nodular regions of inflammation are regions of necrosis that also contain suspected, negatively staining, yeast or algal organisms. Many multinucleated cells surround the regions of necrosis, and the suspected organisms are also within the cytoplasm of many macrophages. Multiple small to moderately sized aggregates of lymphocytes and plasma cells are within the kidney.
Discussion:
The genus Prototheca entails species of achlorophyllous, unicellular, saprophytic, aerobic algae closely related to Chlorella spp. These algae are ubiquitous in the environment and may be isolated from fresh and marine water, soil, mud, tree sap, and sewage. Prototheca reproduce asexually by internal cleavage (endosporulation), resulting in the formation of 2 to 20 small endospores within the sporangium, which expand until they are released when the sporangium ruptures.
In human patients, protothecosis has 3 manifestations: i) dermatitis (comprising more than half of reported human cases), ii) olecranon bursitis, and iii) disseminated or systemic infection. Most lesions of the skin and olecranon bursa result from local traumatic inoculation. Human systemic infections are almost uniformly associated with immune compromise, occurring most commonly with anticancer therapy, organ transplantation, or clinical AIDS, and most commonly affect the skin and subcutis, alimentary tract, peritoneum, blood, and spleen.
Canine cases of protothecosis are uncommon but are increasingly recognized worldwide. A recent review of canine protothecosis identified 31 canine cases in the primary literature, largely arising from the United States.
In contrast to the human disease,canine protothecosis typically involves a broadly disseminated infection, particularly involving the colon, nervous system, and eyes, as well as the heart, kidneys, skeletal muscle, and liver. Frequent involvement of the colon makes colitis (with or without hematochezia) a common presenting complaint; other common presenting complaints include neurologic disease, blindness, and less frequently, polyuria and polydipsia.
Little is known regarding the pathogenesis of canine protothecosis. In human cases the predominance of uncomplicated cutaneous lesions suggests that direct traumatic inoculation is most likely; however, the paucity of cutaneous lesions in canine patients with disseminated disease suggests this is less likely. Most sources suggest the colon as the most likely principle site of infection, resulting in chronic granulomatous colitis and eventual dissemination of the alga to other sites of predilection. Immune dysfunction is often posited as a contributor to this pathogenesis in order to account for its sporadic occurrence, as well as to explain the possible predisposition of collies and boxers.
Protothecosis carries a grave prognosis in the canine patient. Stenner et al identified only 2 cases of canine protothecosis that survived the infection out of 31 cases reviewed. In contrast, the same review found only 2 human cases in which death was attributable to protothecosis. Stenner et al also described 17 cases of protothecosis in dogs from Australia, including 6 cases that underwent treatment. Two dogs that were presented with colitis without any indication of disseminated infection were treated with amphotericin B, with survival times noted as 12 and 17 mo and no indication of dissemination of infection (specific causes of death were not indicated). One dog presenting with colitis and later developing nervous and ocular disease was treated with amphotericin B and itraconazole, and survived to the time of publication. Three dogs were treated with ketaconazole; 2 of these animals failed to improve with therapy and were euthanatized, and 1 was euthanatized before adequate time had elapsed to assess therapeutic efficacy.
Arguments may be made that the poor prognosis associated with protothecosis could be related to the late stage of diagnosis in the progression of disease and that early detection of infection might permit earlier and more effective treatment before extensive dissemination. However, early differential diagnosis of protothecosis is complicated by the numerous other causes of chronic diarrhea and by the very small likelihood of Prototheca infection. Unfortunately, Prototheca frequently is not considered as a differential diagnosis until seen by referral specialists, or until the development of secondary lesions of dissemination to the brain or eye. Even with the development of granulomatous endophthalmitis there are numerous more likely differential diagnoses in the dog, including Blastomyces dermatitidis and Cryptococcus neoformans, more rarely Coccidiodes immitis or Histoplasma capsulatum infection. It is usually the development of ocular and/or nervous dysfunction in the face of chronic colitis that directs the clinician toward a diagnosis of disseminated protothecosis. A better understanding of the factors that contribute to the development of this disease might provide early indicators of Prototheca spp. infection.
The idiosyncracies of canine protothecosis, including methods of transmission, the tendency towards broad systemic dissemination, predilection for specific organs, and possible differential susceptibility of boxers and collies provide many questions to be answered on this disease.
Considering that many human cases arise in North America, it is important to consider protothecosis as a rare but important differential diagnosis for cases of hemorrhagic colitis with onset of multisystemic disease in the canine patient.
Vince AR, Pinard C, Ogilvie AT, Tan EO, Abrams-Ogg AC. Protothecosis in a dog. Can Vet J. 2014 Oct;55(10):950-4. Erratum in: Can Vet J. 2021 Jun;62(6):590. PMID: 25320382; PMCID: PMC4187369.
Patient outcome:
Immediate post-operative condition was significantly improved, the patient demonstrated increased activity levels, appetite and overall improved comfort. She did experience moderate regurgitation which resolved with administration of prokinetic therapy and a nasogastric tube to remove excess fluid from the stomach. She was released to her owners care approximately 48 hours after surgery.
At the time of her 2-week recheck, the owners reported a significant improvement in her comfort, activity, and demeanor.
Approximately 4 months post-op, the owners were contacted for follow up and reported that Sandy had been humanely euthanized. No specific cause for her decline was discussed. It is suspected that due to the diagnosis of Prototheca and the inability to safely remove all abnormal tissue at the time of surgery, that her growth returned and negatively affected her quality of life.
A very special thanks to Four County Animal Hospital for sharing patient details and allowing for an in-depth discussion of their patient.
A special thank you to Dr. Raphael Repellin for collaborating on this case with advanced imaging details and surgical expertise.
September's Case of the Month - 2023
Sonographer: Kara Woody DVM
Importance of Echocardiogram Follow-up for positive ProBNP Results in Felines
2 case examples
Patient Information:
Patient 1
Age: 9 years Gender: Neutered Male
Breed: DSH Species: Feline
Patient 2
Age: 9 years Gender: Spayed Female
Breed: DSH Species: Feline
History:
Littermates/housemates presented for routine dental procedure. Snap ProBNP was performed as part of a pre-anesthetic laboratory panel. Abnormal results were obtained for both patients. Neither patient was displaying any clinical signs of heart disease and no murmurs or arrhythmias were present on exam. Echocardiogram was recommended.
Ultrasonographic Findings:
Patient 1
52 images including 2D, M-mode, color flow and Doppler imaging are available for review. The left ventricular wall is asymmetrically hypertrophied, especially the free wall with regions of remodeling and irregularity (IVSd 4.2, LVPWd 7.5, normal under 6 mm). There is a diffusely hyperechoic endocardium consistent with fibrosis. The systolic function is decreased (fractional shortening 31%, normal over 35%). The E and A waves are summated making assessment of diastolic dysfunction difficult. The papillary muscles are mildly remodeled. The left atrium is severely dilated (LA:Ao 2.64, normal under 1.6; LA diameter 28.6 mm, normal under 16). Spontaneous echo contrast visible but no obvious thrombus. Mild central MR due to annular stretch. Moderator band in LV lumen.
The right ventricle is also affected, with diffuse fibrosis and remodeling. Mild RA dilation with mild TR. Blood flow through the RVOT and LVOT is low normal velocity. Trace pulmonic regurgitation. No pericardial or pleural effusion. No obvious cardiac tumors.
LA:AO short axis view of Patient 1 demonstrating severe left atrial dilatation
“Smoke” (spontaneous echo contrast) noted in the left auricle in an optimized view for this area in Patient 1.
M-Mode left ventricle short axis of Patient 1 demonstrating increased thickness of the left ventricular posterior free wall in diastole.
Patient 2
41 2D, M-mode, color flow and Doppler images are available for review. The left ventricular wall is normal in dimension (IVSd 4.7, LVPWd 3.8, normal under 6 mm). There is a diffusely hyperechoic endocardium consistent with age-related fibrosis. Minimal remodeling. The papillary muscles are hyperechoic. The left atrium is normal in size (LA:Ao 1.34, normal under 1.6; long axis 13.3 mm). Systolic function appears adequate (fractional shortening 52%).
The right atrium is normal in size. The right ventricle appears normal. The mitral valve is normal in structure and mobility with no mitral regurgitation. The tricuspid valve appears normal in structure and mobility with trace tricuspid regurgitation. Blood flow through both the LVOT and RVOT are normal in velocity. Trace pulmonic regurgitation is identified.
LA: AO short axis view of the Patient 2 demonstrating a normal ratio.
M-mode left ventricle short axis of Patient 2 demonstrating normal ventricular wall thickness in diastole.
Echocardiogram Interpretation:
Patient 1
The finding of severe atrial enlargement in the face of moderate LV wall hypertrophy and systolic dysfunction is most consistent with hypertrophic cardiomyopathy developing a restrictive phenotype, however some historical infectious or inflammatory insult to the myocardium cannot be definitively ruled out. According to the most recent classification this is called non-specific cardiomyopathy. The biatrial dilation is causing insufficiency of both AV valves, and systolic dysfunction has developed.
Patient 2
No significant abnormalities noted. Trace tricuspid and pulmonic regurgitation.
Recommendations:
Patient 1
In view of the severe atrial enlargement, this patient is at high risk for thromboembolic events regardless of medications and this should be expressed to the owner (monitor for neurologic change, acute paralysis/lameness, etc).
Monitoring of sleeping breathing rates at home is highly recommended as the best way to screen for development of congestive heart failure at home.
Oral medications which are required lifelong:
Antithrombotic medication clopidogrel (Plavix) 75 mg tablets; give ¼ tab orally once daily (NOTE: this medication is very bitter on the cut edges so placing in a gel capsule can help).
Pimobendan (off label use) although starting this could be delayed until heart failure develops: 625 mg PO q12h.
A recheck echocardiogram is recommended in 6 months to assess for progression.
Patient 2
Given these findings, no medications are indicated. It is important to note that phenotypic HCM can develop at any phase of life in cats (particularly in this predisposed breed), and often does not accompany a heart murmur or physical examination abnormalities. Periodic screening is ideally recommended in all cats.
No cardiac contraindication for general anesthesia at this time.
Recommend recheck echocardiogram in 1 year to assess for development of disease, sooner if a murmur/gallop or clinical signs develop in the interim.
Discussion:
These two cases illustrate why performing screening echocardiograms on patients with abnormal proBNP results is so important. These patients are littermates and reside in the same household. Both are asymptomatic with no heart murmurs or other abnormalities on physical exam; however, their heart structure is drastically different. The male patient (Patient 1) has significant cardiac disease and is at high risk of thromboembolic disease, while the female patient (Patient 2) is basically normal. Assumptions cannot be made based on proBNP findings alone until further testing (ideally echocardiogram) is performed. This is illustrated nicely in this particular pair. ProBNP testing has been evaluated in multiple studies and is generally accepted as a useful “screening” modality in felines especially prior to anesthesia since occult cardiomyopathy can be common in this species. Negative test results have generally been accepted as reliable for ruling out significant cardiac disease. However, a recent paper did show a higher false negative rate when screening healthy cat populations than previously reported, so it is important to remember that a negative result does not definitively rule out heart disease. Furthermore, false positives can also occur and are often complicated by comorbidities common in geriatric felines such as renal failure or hypertension. It is also unclear if proBNP testing can detect cardiac disease prior to echocardiographic changes, so serial echocardiograms could also be considered in patients with abnormal proBNP results even if echocardiographic changes are not presently noted.
Sonographer: Kara Woody, DVM
Reference: Lu, et al. Point of Care N Terminal Pro-B type natriuretic peptide assay to screen apparently healthy cats for cardiac disease in the general practice.. J Vet Intern Med. 2021;35:1663–1672
Thank you to Dumfries Animal Hospital for collaborating with us on these interesting cases and Simon Swift, MA, VetMB, CertSAC, DipECVIM-CA (Cardiology), MRCVS for cardiology interpretation and comments on proBNP testing.
August's Case of the Month - 2023
Sonographer: Anne Desrochers DACVIM
Congenital Cardiac Disease in a Dog
Patient information:
Age: 1 year old
Species: Canine
Breed: Mixed Breed
Gender: Female – 9Kg
History:
Patient presented for failure to thrive and recent development of abdominal distension. A grade 5/6 systolic murmur was detected on auscultation. Heartworm test was negative. Thoracic radiographs were declined.
Echocardiogram interpretation:
The tricuspid valve was thickened especially the septal leaflet and the mural leaflet appeared tethered with moderate to severe tricuspid regurgitation. Right atrial and ventricular dilation were present with hypertrophy of the right ventricular free wall. The pulmonic valve was thickened with significant pulmonic regurgitation and pulmonary artery hypoplasia was evident. RV outflow tract velocities were elevated with a pressure gradient of up to 135 mmHg (severe over 80). Severe ascites was visualized.
Diagnosis:
Severe pulmonic stenosis and tricuspid valve dysplasia were present with secondary right ventricular hypertrophy and dilation, heart failure and moderate tricuspid regurgitation.
Images #1 and #2. Left - right parasternal long-axis 4-chamber view showing the right ventricle (RV) and atrium (RA) enlargement compared to the LV and LA, and hypertrophy of the right ventricular free wall (asterisk). Right - color flow Doppler showing the significant tricuspid valve regurgitation.
Image #3. Right parasternal short-axis view showing the significant thickening of the free wall and spectal leaflets of the tricuspid valve (arrows).
Image #4. Right parasternal short-axis view showing the pulmonic valve thickening (arrow), color flow Doppler of the pulmonic regurgitation and proximal narrowing of the pulmonary artery (PA).
Therapeutic recommendations:
Aggressive medical therapy for congestive heart failure was recommended as well as referral for balloon valvuloplasty as this procedure can improve longevity.
Outcome:
The client was informed that once heart failure is present, the outcome with balloon valvuloplasty is considered guarded and often prolongs survival by only 1 to 2 years. Due to the severity of the pet’s condition and poor long-term prognosis, the client opted for humane euthanasia.
Comments:
The literature suggests that fewer than 1% of dogs are affected by congenital heart disease. In two publications, pulmonic stenosis (PS) was the most frequently detected defect when combined cardiac malformations were present - 59.24% in 211 cases and 63.19% in 144 dogs. The combination of pulmonic stenosis and tricuspid dysplasia appears rare, being reported in only 3 out 976 dogs (0.3%) in one study.
Retrospective Review of Congenital Heart Disease in 976 dogs. Oliveira P et al. J Vet Intern Med 2011 May-Jun;25(3):477-83.
Epidemiological study of congenital heart diseases in dogs: Prevalence, popularity, and volatility throughout twenty years of clinical practice. Brambilla PG et al. PLoS One 2020 Jul 27;15(7):e0230160.
Special thanks to Dr. Simon Swift (DipECVIM - cardiology) and the staff at Banfield Urbana Pike for their help with this case.
July's Case of the Month - 2023
Sonographer: Meredith Adams, DVM
Subcutaneous Foreign Body
Signalment:
Age: 8 year old
Gender: Neutered Male
Species: Canine
Breed: Doberman
History:
Abdominal ultrasound was requested for patient due to persistent fever, lethargy, anorexia and weight loss, and polydipsia. Previously performed thoracic and abdominal radiographs and bloodwork were all unremarkable.
With patient in dorsal recumbency for abdominal ultrasound, a subtle flat, firm, fluctuant swelling was noted over the right caudolateral ribs.
Ultrasonographic findings:
The subcutaneous tissue over the right caudal ribs is severely hyperechoic and surrounds pockets of echogenic fluid. There is a thin hyperechoic linear object (at least 4.4cm long) that extends from within a fluid pocket to between the 9th and 10th rib and penetrates into the abdominal cavity. Some free gas is seen within the fluid pocket.
Mesentery throughout the right cranial abdomen is diffusely hyperechoic.
The remainder of the full abdominal ultrasound was unremarkable.
Abdominal ultrasound interpretation:
Subcutaneous fluid pockets - the findings are moderate and consistent with abscess formation
Linear object - the findings are moderate and suggestive of a foreign body penetrating through the subcutaneous tissues and into the abdominal cavity
Mesentery - the findings are moderate - DDx: peritonitis - inflammation vs. paraneoplastic reaction vs. infectious vs. fibrosis vs. other.
Provided Recommendations:
An aspirate of a subcutaneous fluid pocket was recommended and performed. Purulent fluid was obtained confirming the presence of an abscess
Consider submitting aspirate for culture and sensitivity
Recommend exploratory laparotomy to fully evaluate the abdomen and foreign body and potentially resolve with surgical intervention.
Outcome:
Surgery was performed to remove the foreign body via the abscess over the right caudal ribs. A wooden linear object (large toothpick or similar) was removed. An exploratory laparotomy was not immediately performed. Though there were no visible wounds, external penetration was suspected due to the orientation of the pointed part of the foreign object being deeper into the subcutaneous tissues. The patient made a full recovery following surgery.
Discussion:
Ultrasound can be used to routinely assess internal abdominal structures, but can also assess more superficial soft tissue structures such as abnormal subcutaneous and muscle tissues. While differentials for this patient initially included other causes of fever of unknown origin that may be commonly identified via abdominal ultrasound, an extra-abdominal abnormality was identified using the same imaging modality in an unexpected location.
Special thanks to the staff at Varina Veterinary Clinic for collaborating on this case.
June's Case of the Month - 2023
Sonographer: Emily Evans, BVM&S
Confirmation of Rodenticide Toxicity
PATIENT INFORMATION:
Age: 7.5 years
Gender: Male
Species: Canine
Breed: Pitbull
Weight: 77lbs
HISTORY:
The patient presented for lethargy. There was an imprecise history given which included possible ingestion of multiple toxins from a garden shed (Potentially ingested agents - Diphacinone, bromethalin, pyrethroids, weed killer, possible other “garage” contents.) The exact timing of ingestion provided by the owner was unclear.
On initial physical examination the patient was dull and had a large caudal abdominal mass/bladder. There was concern for a bleeding tumor or other caudal abdominal mass on physical exam and radiographs.
ADDITIONAL DIAGNOSTICS:
Radiographs - Decreased serosal detail, mass effect in the caudal abdomen.
PCV/TS -initial presentation 36%/6.8 repeat evaluation 23%/4.8
ULTRASOUND FINDINGS AND IMAGES:
Spleen - Normal size(2.0cm), shape, and echogenicity. There is a heterogenous well defined capsule altering hypoechoic nodule in the spleen(2.0x2.6cm) The splenic nodule is vascular.
Liver -Normal size, shape and moderately coarse echogenicity. No focal lesions are appreciated. The gall bladder is moderately distended with normal anechoic and hyperechoic unorganized dependent bile that is not resulting in obstruction. No common bile duct dilation is seen.
Serosal Surfaces- There is a mild-moderate amount of free fluid in the abdomen. Fat and tissue surrounding the prostate is severely heterogenous and hyperechoic. Mesentery throughout the abdomen is diffusely hyperechoic.
Kidneys- Normal size (Lt/Rt = 6.9/7.4 cm) and shape with normal corticomedullary dimensions. No pyelectasia visualized. There is a moderate amount of hypoechoic heterogenous avascular change in the retroperitoneal space bilaterally with a mild amount of free fluid.
Prostate- Severe generalized enlargement with hyperechoic coarse echogenicity and multifocal anechoic small cysts throughout. No mineralization or focal lesions. (LxDxW - 9.7x5.0x5.4cm)
Lymph Nodes - The medial iliac and sublumbar lymph nodes are mildly enlarged with rounded shape having homogenous mildly hypoechoic echogenicity. (Lt/Rt: 1.2/1.7cm, 0.7cm)
Urinary Bladder- The bladder is mildly distended with mildly echogenic urine and the bladder walls are mild-moderately thickened(10.2mm) and irregular in contour and thickness. No overt obstruction, uroliths, or neoplasia noted.
DIAGNOSIS:
Multiple sites of suspected hemorrhage and hematomas(ascites, retroperitoneal change, splenic lesions, urinary bladder and mesenteric changes) secondary to anticoagulant rodenticide ingestion.
Prostatic enlargement coupled with ascites and mesenteric change gave the appearance of a caudal abdominal mass. The prostatic change is likely secondary to prostatitis or benign prostatic hyperplasia in this intact individual.
CASE OUTCOME:
No samples were collected from this patient due to concerns for bleeding diathesis. The patient was transferred to ER for a transfusion and vitamin K therapy was initiated.
Follow up with the owners 5 days after the initial presentation, the patient was said to be doing well.
PROGNOSIS/DISCUSSION:
Recheck ultrasound 30 days after finishing was recommended to reassess changes.
Neuter was recommended to address prostatic enlargement.
DISCUSSION:
Abdominal ultrasound can be utilized in cases of suspected or known anticoagulant rodenticide toxicity to assess for presence of and extent of internal hemorrhage. This patient had no external signs of a bleeding diathesis but multiple intra abdominal signs which were concerning for hemorrhage and supported the diagnosis of anticoagulant rodenticide ingestion. This evidence aided in the initiation of appropriate therapy.
References:
Merola, V. (2002). Anticoagulant rodenticides: Deadly for pests, dangerous for pets. Veterinary Medicine.
Baranidharan GR, AP Nambi, S Kavitha, PS.Thirunavukkarasu , P Sridhar, H Yamini and S Muthuvel, 2014. Anticoa- gulant rodenticide toxicity and secondary haemostatic disorder in a dog. Inter J Vet Sci, 3(1): 37-39. https://url.avanan.click/v2/___www.ijvets.com___.YXAzOnN2cDphOmc6N2NiY2E1NzQ2MWJhNTFjZjRiNDgxNjIyZmEyY2E4MWY6NjpjZWJmOjM2NmE0M2FhOWViOTcxZjg5MDZkYWE2NGVjOTJmYWM3NTFjMmE1N2UwNTk4NDUxODgxY2Y3ZWRmNWIyMGNhYzY6dDpU
Sheafor, S.E.; Couto, C.G.: Anticoagulant rodenticide toxicity in 21 dogs. JAAHA 35 (1):38-46; 1999
RT O’Brien, E F WoodVet Radiol Ultrasound Jul-Aug 1998;39(4):354-6 Urinary bladder mural hemorrhage associated with systemic bleeding disorders in three dogs
Thank you to the veterinarians and staff of Varina Veterinary Clinic for collaborating with us on this case.
May's Case of the Month - 2023
Sonographer: Mallory Repellin, DVM
Transitional Cell Carcinoma in a Canine
Patient information:
Age: 7 years
Gender: Spayed Female
Breed: Border Collie Mix
Species: Canine
History:
Chronic hematuria. Urinary cultures have been negative. Patient is not responsive to antibiotics.
Patient is also concerned to have osteoarthritis or soft tissue injury to the left rear limb, she has been toe-touching to non-ambulatory on this limb recently.
Ultrasonographic findings:
The bladder is moderately distended with anechoic urine and is of relatively normal contour and thickness. There is a 2.8 x 2.3 cm hyperechoic lobular mass originating from the mid-ventral bladder wall. Positive color doppler noted within the mass.
Caudal right rib mass measuring 2.4 x 2.9 cm (sagittal), which appears hypoechoic with multifocal regions of mineralization. Approximately 9-12th rib.
Abdominal ultrasound interpretation:
Bladder Mass - the findings are moderate to severe - DDx: Tumors of the urinary bladder are uncommon in dogs and rare in cats. Transitional cell carcinoma (TCC) is the most common primary tumor of the urinary bladder in both species. Other differentials include squamous cell carcinoma, leiomyosarcoma, leiomyoma, and rhabdomyosarcoma or benign bladder polyp. The bladder may also be invaded by prostatic neoplasia or metastatic disease (e.g., hemangiosarcoma, lymphoma). Bacterial cystitis and urolithiasis are common differentials for the clinical signs seen, and a rare but important differential diagnosis for mass lesions is benign polyps of the urinary bladder.
Rib Mass - the findings are moderate- DDx: chondrosacroma, osteosarcoma, soft tissue sarcoma, other neoplasia, less likely granuloma, abscess, cyst
Images:
Additional tests:
Fine needle aspiration of the suspected rib mass was performed with cytologic interpretation.
Cytology report:
The diagnosis of a carcinoma is definitive (100% confidence). Based on the morphology of these epithelial cells with occasional large pink secretory vacuoles, a clinical suspicion for metastatic transitional cell carcinoma is warranted (LeBlanc CJ, Roberts CS, Bauer RW, Ryan KA. Firm rib mass aspirate from a dog. Vet Clin Pathol. 2004;33(4):253-6.).
The slides are moderately to highly cellular and consist of a large amount of cellular debris suggesting necrosis, few to many red blood cells and a nucleated cell population predominated by round to polygonal cells found in cohesive clusters. These cells have a small amount of very basophilic cytoplasm that surrounds a central, round nucleus with a coarsely-stippled chromatin pattern and 1-3 prominent nucleoli. Anisokaryosis is moderate; binucleation is commonly noted. Occasionally these cells contain one to two large cytoplasmic vacuoles that contain an abundant amount of thick, pink secretory material. Few leukocytes in proportions consistent with peripheral blood are also present.
Several clusters of polygonal cells with large round to oval nuclei
Recommendations:
Referral to a veterinary surgeon and/or oncologist for further diagnostics (CT scan) and therapy is highly recommended.
Thoracic radiographs (3-view, metastasis check) are recommended.
Discussion:
Invasive transitional cell carcinoma (TCC) is the most common form of canine urinary bladder cancer affecting tens of thousands of dogs worldwide each year, and the prevalence appears to be on the rise. Most TCCs are intermediate to high-grade papillary infiltrative tumors; superficial, low-grade tumors are uncommon. TCC is most often located in the trigonal region of the bladder. In one large study of 102 dogs with bladder TCC, more than half of the patients had concurrent urethral involvement and about a third of male dogs had concurrent prostatic disease.1 Distant metastases are typically present in about 20% of cases at diagnosis and are associated with a worse prognosis. More than 50% of dogs with TCC have distant metastases by the time of death2. Apart from regional lymph nodes and lungs, the metastatic spread can be seen in liver, spleen, kidneys, bones, adrenal glands, heart, brain, and skin. The mean age at diagnosis is 9 to 11 years, with females being affected more commonly.
Patient outcome:
Radiographs of rear limb showed a left 4th digit distal phalanx fracture with concern for disease infiltration to the bone.
The patient had a scheduled consultation with a veterinary oncologist to discuss therapy options for metastatic transitional cell carcinoma. Approximately 1 week following ultrasonographic findings, the patient experienced an episode of collapse and was unable to recover. She was taken for emergency care where the possibility of metastatic lesions to the spine were suspected based on current clinical signs. Owner declined further therapy options and elected for euthanasia at this time.
Sonographer: Dr. Mallory Repellin
Special thanks to Wheaton Animal Hospital and Dr. Casey Leblanc at Eastern VetPath.
April's Case of the Month - 2023
Sonographer: Kara Woody, DVM
Ovarian Teratoma in an Intact Female Rottweiler
Patient Information:
Age: 7 years
Gender: Intact Female
Breed: Rottweiler
Species: Canine
History:
Patient presented with increased urination frequency and hematuria. Lateral abdominal radiographs were performed and a large mineralized mass was visualized caudal to the tail of the spleen.
Lateral radiographs showing rounded mineralized mass caudal to spleen.
Photo Credit: Ridge Lake AH
Ultrasonographic Findings:
The left ovary was severely enlarged (7.8x5.0cm) and rounded in shape with a mixed echogenicity with large cystic cavitations and focal areas of mineralization. Vascularity was minimal on Doppler exam. The uterus and right ovary appeared normal. No other areas of metastasis were visualized within the abdomen.
Ultrasound image of large mixed echogenic left ovarian mass with areas of mineralization.
Abdominal Ultrasound Interpretation:
Left Ovarian mass-the findings are severe-DDX: epithelial tumors (cystadenoma vs adenoma vs adenocarcinoma) vs teratoma vs sex chord tumor vs mesenchymal tumor vs metastatic tumor
Recommendations:
Ovariohysterectomy was recommended with histopathology of the left ovarian tumor. 3 view thoracic radiographs had already been performed and were negative for metastasis. Pre-surgical laboratory work was within normal limits.
Surgical findings:
Ovariohysterectomy was performed with successful removal of left ovarian tumor. The tumor was observed to have areas of skin and hair development as well as large cystic areas during sectioning. No other abnormalities were found in the uterus or right ovary.
Mass at time of ovariohysterectomy.
Photo Credit: Ridge Lake AH
Biopsy Results:
Microscopic description: Markedly compressing the surrounding ovarian follicles and stroma is a nonencapsulated, well-demarcated, nodular, and multilocular mass, composed of various types of well-differentiated and haphazardly arranged tissue derived from the ectoderm and mesoderm. Separating large bundles of neuroparenchyma, scattered ganglion cell bodies are moderate amounts of fibroadipose tissue that surround markedly ectatic/cystic hair follicles, which contain abundant lamellar keratin and hair shafts. Surrounding the hair follicles are few lobules of apocrine glands, and coalescing aggregates of lymphocytes, plasma cells, and scattered pigment laden macrophages.
Microscopic findings: Well differentiated teratoma.
Histopathology Image: Hair follicles evident as well as keratin formation.
Photo credit: Antech Diagnostics
Discussion:
Teratomas are uncommon, but have been described most often in the bitch. They are tumors that originate from at least 2 of 3 germinal layers (ectoderm, endoderm and mesoderm) Therefore, a combination of tissues such as hair, skin, nervous tissue, bone, and teeth can be found within the tumors. While they can become quite large, they are most often benign and removal is curative. Malignant tumors can occur uncommonly.
Patient Outcome:
The patient recovered uneventfully from surgery and continues to do well. Prognosis is excellent in this case.
Sonographer: Kara Woody, DVM
Thank you to Ridge Lake Animal Hospital for collaborating with us on this interesting case and Antech Diagnostics for the histopathology images and report.
March's Case of the Month - 2023
Sonographer: Anne Desrochers, DACVIM
Congenital Cardiac Defects in a Cat
Patient Information:
Age: 4 years old
Species: Feline
Breed: DSH
Gender: Male
History:
Feline patient from an animal rescue. Clinically asymptomatic for heart disease. A grade 3/6 systolic murmur was detected on auscultation. Pro-BNP was elevated at 436pmol/L (N - <100).
Echocardiogram interpretation:
Complex congenital heart disease. There appeared to be a second chamber in the dorsal left atrium which could be a supravalvular mitral stenosis or a cor triatriatum sinister. The right ventricle had a very abnormal papillary muscle/ridge that seemed to divide the right ventricle into a high pressure proximal chamber and a lower pressure distal chamber consistent with a double chamber right ventricle. There was also concern that a small VSD was present.
Diagnosis:
Double chamber right ventricle, CTD/supravalvular mitral stenosis with po
Image 1. Right parasternal long-axis view showing the normal left ventricle (LV) and atrium (LA) and the double chamber right ventricle (RV1 and RV2).
Image 2. Right parasternal short-axis view showing the normal left ventricle (LV) and the double chamber right ventricle (RV1 and RV2).
Image 3. Right parasternal long-axis view showing the 2nd chamber dorsal to the left atrium and suspected supravalvular mitral stenosis or cor triatriatum sinister (arrow).
Monitoring and therapeutic recommendations:
The patient had reached 4 years of age with no clinical signs and RV hypertrophy. No treatment was clearly indicated but beta blockers such as atenolol or propranolol could be considered. While balloon dilation of the RV obstruction could be attempted, it is very muscular so unlikely to respond. Referral to a board-certified cardiologist for full evaluation and a repeat echocardiogram in 6 months were recommended.
Outcome:
Due to additional health concerns and a stable cardiac condition, the rescue opted to not pursue referral at that point.
Special thanks to Dr. Simon Swift (DipECVIM - cardiology) and the staff at Loudoun Cats Care for their help with this case!
February's Case of the Month - 2023
Sonographer: Meredith Adams, DVM
Linear Intestinal Foreign Body in a Cat
Signalment:
Age: 1 year old
Gender: Neutered Male
Species: Feline
Breed: DSH
History:
Abdominal ultrasound was requested to evaluate patient for lethargy and anorexia. Bloodwork revealed a leukocytosis of 31.6K with a neutrophilia (26.7k), monocytosis (2.4k), basophilia (0.2K) and eosinophilia (0.8K). The patient’s hematocrit was also elevated at 51%. His chemistry panel showed a mildly elevated ALT (143U/L [12-140]) and GGT (24 [0-4U/L]). Abdominal radiographs were unremarkable.
Ultrasonographic findings:
There was linear foreign material seen from the level of the ileocecocolic junction (ICCJ) extending within the lumen of the ileum and through a large portion of the jejunum causing moderate to severe plication of the small intestine. The origin of the foreign material was not determined, but it was not visualized in the duodenum or pylorus. The small intestine had normal layering and thickness (Duodenum 2.5mm; Jejunum 2.3-2.6mm). The colon had normal wall thickness (1.1mm) and layering throughout. The stomach was empty and collapsed with normal rugal folds and layering.
Multiple mesenteric lymph nodes were mildly enlarged (0.6cm depth) with rounded shape having homogenous hypoechoic echogenicity.
No free fluid or free gas was noted in the abdomen.
Arrow showing hyperechoic linear foreign body in the lumen of the jejunum:
Hyperechoic linear foreign body in the ileum at the level of the ICCJ:
Hyperechoic linear foreign body in the lumen of the jejunum causing small intestinal plication:
Abdominal ultrasound interpretation:
Intestines - the findings are moderate and suggestive of an obstructive linear intraluminal intestinal foreign body. Adhesions or evidence of peritonitis were not appreciated on ultrasound, but this does not rule it out.
Lymph nodes - the findings are mild - DDx: infiltrative neoplasia (lymphoma vs. mast cell vs. other) vs. IBD vs. infection vs. reaction vs. metastatic neoplasia
Recommendations:
Exploratory laparotomy was recommended to surgically remove the foreign body. Though lymphadenopathy was suspected to be reactive secondary to the foreign body, taking biopsies of mesenteric lymph nodes could also be considered.
Outcome:
Exploratory laparotomy was performed. A linear foreign body was located throughout the jejunum and ileum that was embedded in the wall of the intestine and beginning to perforate. An intestinal resection and anastamosis was performed. The patient made a full recovery from surgery and is doing well.
Discussion:
Patients with linear foreign bodies may present with acute severe or vague mild clinical signs including lethargy, hyporexia/anorexia, vomiting, and signs of dehydration. Peristaltic waves cause the intestine to gather around the foreign material resulting in intestinal plication. The mesenteric border of the intestine is most at risk of perforation due to the linear material becoming taut and cutting into the mucosa. Rapid diagnosis and surgical intervention can help avoid perforation and septic peritonitis from occurring. Physiologic and anatomic ileus are not always easily differentiated on abdominal radiographs. Abdominal ultrasound can more definitively diagnose this condition.
Reference:
Fossum, Theresa Welch, et al. Small Animal Surgery. 2nd ed., Mosby 2002.
Sonographer: Dr. Meredith Adams
Special thanks to Dr. Olenic and the staff at Varina Veterinary Clinic for collaborating on this case.
January's Case of the Month - 2023
Sonographer: Dr. Emily Evans
Ureteral Papilla Obstruction with Spontaneous Resolution in a Cat
PATIENT INFORMATION:
Age: 11yo
Gender: Female Spayed
Species: Feline
Breed: DSH
Weight: 6.7lbs
HISTORY:
Past Medical History:
- constipation, managed with diet & Miralax
-R hip luxation 9/10/2020
-Cherry Eye
Historic lab findings 2020- SDMA 11 ug/dL, CREAT 1.0 mg/dL, BUN 16 mg/dL, UA USG 1.024
Presented Mid November 2022 with reduced appetite.
Labs
11/11- SDMA 16ug/dL, CREAT 3.3mg/dL, BUN 49mg/dL, UA USG 1.014
12/13- SDMA 14ug/dL, CREAT 3.0mg/dL, BUN 56mg/dL
1/17- SDMA 22ug/dL, CREAT 3.1mg/dL, BUN 51mg/dLObjecti
INITIAL ULTRASOUND FINDINGS:
Both kidneys were found to have changes suggestive of CKD(coarse mild to moderately hyperechoic renal cortices which were disproportionately large). There was mild-moderate loss of the corticomedullary junction distinction as well as lobar scalloping. The renal pelvis was hyperechoic bilaterally. There were a few small thin-walled anechoic cortical cysts seen throughout both kidneys.(up to 0.2cm)(Lt/Rt = 3.8/3.7 cm). No significant pyelectasia was visualized.(<1.5mm)(Normal - up to 0.4mm*)
The left ureter is mildly dilated from the kidney to the papilla. (up to 2.6mm)
There was a severely hyperechoic, minimally shadowing, rounded structure in the left papilla.(1.7x1.8mm)The bladder was moderately distended with anechoic urine and of relatively normal contour and thickness No neoplasia or other uroliths noted.
Other ultrasound findings - mild hepatopathy, mild pancreatitis and mild lymph node changes.
DDX:
Hyperechoic rounded structure at left ureteral papilla - the findings were moderate - DDx: plug vs. poorly shadowing mineralization vs. emerging neoplasia vs. historic fibrosis/scar/stricture vs. ureteritis
Ureteral dilation - the findings are mild -DDX: ureteral obstruction acute vs. chronic vs. historic (sludge/plug vs. urolith vs. stricture vs. neoplasia vs. other) vs. ureteritis
Kidneys - the findings are moderate - DDX:
a) Chronic nonspecific change - (chronic glomerulonephritis vs. amyloidosis), chronic interstitial nephritis, chronic nephritis. In cats, the loss of corticomedullary distinction is not unusual with chronic renal disease as interstitial fibrosis in the medulla renders its echogenicity similar to that of the cortex.
b) Acute renal failure/Nephritis (infectious, GN, toxic, etc.) vs. Acute-on-Chronic renal failure
c) Lymphosarcoma
d) Pyelonephritis
SELECT IMAGES:
Image 1: Maytrix/Calculi plug at the left ureteral papilla/distal ureter- Noted in Mid- November
Image 2: Left ureter just distal to kidney
Image 3- Left Ureter approaching the bladder
Image 4 - Bladder trigone free of obstruction at 30 and 60 days. No evidence of hydroureter
Diagnosis - Distal ureteral/ureteral papilla partial obstruction with associated mild hydroureter
CASE OUTCOME:
We are happy to report this patient spontaneously passed the obstruction and has continued to do well with a healthy appetite. Given the very distal position of the obstruction, lack of significant pyelectasia(indicating likely a partial or resolving obstruction) and the improvement in the patient’s appetite, supportive care and acupuncture were continued. The patient was closely monitored for deterioration as aggressive therapy was not going to be pursued. The patient’s appetite continued to improve. Follow up ultrasounds at approximately 30 and 60 days showed complete resolution of the obstruction and no mineralizations/obstructions present in the urinary/urethra bladder.
Her CKD will continue to be monitored. There was a mild improvement in renal function after resolution of obstruction indicating the likely presence of CKD prior to the development of obstruction.
PROGNOSIS/DISCUSSION:
The prognosis is good with some risk of developing future ureteroliths or stricture. It is likely that this patient already had chronic renal disease which likely progressed secondary to the ureteral obstruction. (Other hematological changes associated with CKD were noted on labs)
Clinical signs of partial or unilateral ureteral obstruction in cats may be as subtle as anorexia or pain. Changes in renal parameters in cats showing signs of pain or anorexia should be investigated with abdominal ultrasound.
In some cases ureteral obstruction can result in compensatory hypertrophy of the contralateral kidney (not present in this case). All cases of “Big-Kidney, Little Kidney syndrome” should be investigated for signs of ureteral obstruction independent of uremic state.
References:
Kochin EJ, Gregory CR, Wisner E, et al. Evaluation of a method of ureteroneocystostomy in cats. J Am Vet Med Assoc 1993; 202: 257–260.
Lamb CR. Ultrasonography of the ureters. Vet Clin North Am Small Anim Pract 1998; 28:823-848.
Thank you to our friends at Integrative Veterinary Center of Richmond for including us in the care of this lovely patient.
December's Case of the Month - 2022
Sonographer: Cary Sparkman, DVM
Heartworms in a Young Dog
PATIENT INFORMATION:
Species/Breed: Canine/Chihuahua
Age: estimated just under 1 year old
Gender: Male
Weight: 6.6 lbs
HISTORY:
The patient was adopted about 3 months prior to presentation with no prior history. The patient was presented for lethargy, disorientation (walking into walls), inappetence, coughing and syncopal episodes. An echocardiogram was recommended to rule out a cardiac cause for syncope.
PERTINENT ECHOCARDIOGRAM FINDINGS:
The tricuspid valve appears normal with mild tricuspid regurgitation. The TR velocity is increased suggesting severe pulmonary arterial hypertension and the right ventricle appears subjectively dilated.
Multiple parallel lines are seen in the right atrium and ventricle crossing the tricuspid valve consistent with adult heart worms.
Image 1: Heartworms within the right heart (near field) seen in the right parasternal long axis 4 chamber view
Image 2: Heartworms within the right heart (left screen) seen in the left apical 4 chamber view
Image 3: Heartworms seen falling from the right atrium into the right ventricle in the left parasternal cranial right atrial view
DIAGNOSIS:
In view of the clinical signs and echo findings, caval syndrome is suspected with the adult heart worms migrating from the pulmonary arteries into the right heart causing obstruction and cell lysis. Hemoglobinuria is likely.
There is severe pulmonary hypertension present which is concerning for the longer term.
RECOMMENDATIONS:
Pimobendan (0.2 - 0.3 mg/kg every 12 hours) and sildenafil (1 - 3 mg/kg every 8 hours) should be started and in some cases, this can cause the worms to move back into the pulmonary arteries.
Urgent referral to a specialist center for heart worm extraction is strongly recommended.
Longer term treatment should include doxycycline and prednisolone as per the American Heartworm Association recommendations:
1) Exercise restriction
2) Heartworm prevention
3) Doxycycline at 10 mg/kg BID for 4 weeks
4) Prednisolone 0.5 mg/kg BID tapering every 7 days
4) Melarsomine on day 60, 90 and 91 and repeating the tapering prednisolone regime after injection
5) Test on day 120 and 365
Recommend recheck echocardiogram in 3 months to assess any resolution of the pulmonary hypertension.
FOLLOW UP:
The owner declined referral for heart worm extraction. The patient has been treated medically and is currently doing well.
Sonographer: Cary Sparkman, DVM
Special thanks to Crater Road Veterinary Hospital and Simon Swift, MA, VetMB, CertSAC, DipECVIM-CA (Cardiology), MRCVS with DVMSTAT
November's Case of the Month- 2022
Sonographer: Kara Woody, DVM
Jejuno-Jejunal Intussusception Due to Jejunal Mass
Patient Information:
Age: 8 years
Gender: Spayed Female
Breed: Golden Doodle
Species: Canine
History:
Presented with a two week history of vomiting and regurgitation. Laboratory work is within normal limits.
Ultrasonographic Findings:
There is a jejuno-jejunal intussusception noted in the left cranial abdomen in the mid-jejunum. Blood flow to entrapped mesenteric fat is adequate. There is a hypoechoic mucosal vascular mass with punctate hyperechoic shadowing foci noted at the aboral end of the intussusception measuring 1.5x1.9cm. The rest of the small intestinal loops have normal bowel layering, thickness, and motility. (Duodenum-5.8mm; Jejunum-4.5mm; Ileum-3.9mm). Minimal luminal dilatation is present orad to the intussusception.
Origin of jejuno-jejunal intussusception.
Intussusception in transverse showing normal blood flow to entrapped mesentery.
Jejunal Mass present at the termination of the intussusception
Still image of jejunal mass showing position color uptake on Doppler exam.
Abdominal Ultrasound Interpretation:
Jejuno-jejunal intussusception-the findings are moderate to severe.
Jejunal Mass - the findings are moderate: DDx: adenocarcinoma vs. infiltrative neoplasia (lymphosarcoma vs. mast cell tumor) vs. leiomyosarcoma vs. leiomyoma.
Recommendations:
The prognosis was guarded since the type and behavior of mass was yet to be determined. 3 view thoracic radiographs and resection and anastomosis with histopathology of mass was recommended for optimal treatment plan.
Outcome:
Unfortunately due to guarded prognosis and financial constraints, euthanasia was elected.
Discussion:
Intussusceptions are common in younger animals with 75% present in dogs <1 year of age. Any condition that causes increased motility can predispose. They are often the result of parasitism or enteritis (e.g. parvo virus), but can also be caused by foreign bodies and intestinal neoplasia. Idiopathic cases are also possible. Clinical signs can be acute or chronic and often include vomiting, diarrhea, and weight loss. The most common type of intussusception is enterocolic which accounts for ⅔’s of cases. While radiographs can often increase suspicion of intussusception, ultrasound is the diagnostic modality of choice. Surgical reduction is usually necessary with resection and anastomosis if bowel is found to be compromised. This procedure often carries a good prognosis, provided surgical complications do not occur. In this case, hypermotility was caused by the presence of a luminal jejunal mass likely causing a partial obstruction. This accounts for the unusual location of the intussusception (jejuno-jejunal).
Sonographer: Kara Woody, DVM
Thank you to Shirlington Animal Hospital for collaborating with us on this interesting case.
October's Case of the Month- 2022
Sonographer: Anne Desrochers, DVM DACVIM
Perirenal Pseudocysts in a Cat
Patient Information:
Age: 14 year-old
Gender: Neutered male
Species: Feline
Breed: Domestic short hair
History:
Pet was presented for an annual exam when a possible mass was felt on abdominal palpation. A grade 3/6 systolic murmur was also detected on cardiac auscultation.
Ultrasound Evaluation:
Kidneys: normal size (LT/RT: 4.0/3.9cm) and shape. Both kidneys had coarse moderately hyperechoic renal cortices which were disproportionately large. There was moderate to severe loss of the corticomedullary junction distinction as well as lobar scalloping. The right kidney contained one thin-walled anechoic fluid-filled structure consistent with cystic lesion measuring 0.8x0.9cm in diameter. A mild to moderate (left) to large (right) amount of anechoic fluid was seen surrounding the kidneys in the subcapsular space (see images). No pyelectasia was visualized.
Image #1. Longitudinal view of the left kidney using a high frequency linear probe.
Image #2. Longitudinal view of the right kidney using a high frequency linear probe.
Ultrasound-guided drainage:
Approximately 340mls of clear colorless fluid was removed from the right and 20mls from the left subcapsular spaces. Fluid sample was submitted for cytology and fluid analysis which revealed findings consistent with low cellularity cystic fluid.
Follow up and outcome:
Bloodwork revealed a creatine level of 2.4mg/dl (normal: 0.6-2.4mg/dl) and a BUN of 42mg/dl (normal: 14-36mg/dl) and renal diet was prescribed. A month later, the patient presented for partial anorexia and recurrence of the perirenal effusion was felt palpation. At that point, the owner opted for surgical referral for bilateral laparoscopic capsulectomy. The patient recovered well from surgery besides a slow worsening of the azotemia. But unfortunately, the cat had to be euthanized two months later due to the development of congestive heart failure as a complication of hypertrophic cardiomyopathy and severe left atrial enlargement.
Comments:
Subcapsular perirenal pseudocyst formation can occur at variable stages of renal dysfunction and develop secondary to progressive renal parenchyma contraction which impairs venous or lymphatic drainage resulting in transudation. Resection of the pseudocyst wall is usually effective in eliminating signs but does not stop the progression of the renal disease. The prognosis for cats with pseudocyst formation is related to the degree of renal dysfunction at time of diagnosis.
A retrospective study of 26 affected cats showed that nineteen (73%) affected cats were male. The median age was 11 years. Most presented for abdominal enlargement and had varying degrees of renal dysfunction. Thirteen cats (50%) had bilateral pseudocysts. Eight cats were treated surgically. Cats survived a median of 9 months after surgery and survival was correlated statistically to degree of azotemia at presentation. Percutaneous drainage of pseudocysts was ineffective in controlling long-term fluid accumulation.
Ochoa V et al. Perinephric Pseudocys in the Cat: A Retrospective Study and Review of the Literature. J Vet Intern Med 1999;13:47–55.
Beck JA et al. Perirenal Pseudocysts in 26 Cats. Aust Vet J 200 Mar; 78(3(: 166-71.
Special thanks to the staff at Adam’s Mill Veterinary Hospital for their help with this case.
September's Case of the Month- 2022
Sonographer: Tyler Anderson, DVM
Sonographic Findings of a Right Kidney Mass: A Case of the Month September 2022
Patient Information:
Age: 14 years
Gender: Neutered Male
Species: Canine
Breed: Beagle
History:
An abdominal ultrasound was recommended after a tense abdomen was noted on routine physical examination with a soft tissue mass seen on abdominal radiographs.
Image Interpretation:
Abdominal sonographic findings:
The right kidney is mass-like and severely increased in size (~ 7.3 x 10.2cm). Majority of the kidney is amorphous, having near-complete loss of normal corticomedullary junction distinction. A large anechoic cavitation (~ 4.6 x 5.9cm) is seen having a severely thin wall (Wall thickness: 1.7 mm) at the caudal pole. The cranial pole exhibits a discernible renal cortex with dilation of the diverticuli. The right kidney mass is moderately vascular on color doppler
The left kidney maintained normal sonographic appearance.
A homogenous and mildly hypoechoic liver nodule was also seen in the left liver, measuring ~ 2.0cm.
Sonographic appearance of the right kidney mass. Notice the large, thin-walled anechoic cavitation seen along the caudal pole.
Diagnosis and Sonographic Analysis:
The owner elected to have a nephrectomy performed. A 3 hour surgery was successfully completed by Dr. Neuman, and patient was reportedly BAR and eating shortly after being discharged from the hospital.
Due to the size of the right kidney, a cross section (~ 5.0 x 50 cm) of the kidney was sent to Antech for histopathology.
Images from surgery:
Right Kidney Mass
The large fluid-filled cavitation in the caudal pole can be seen during post-operative dissection.
Histopathology Results:
Received: 5.0 cm x 50 cm tissue.
Description:
The multiple sections of ovary examined had a multinodular malignant neoplastic process consistent with renal tubulopapillary cystadenocarcinoma. It was characterized by neoplastic proliferation of epithelial cells which formed irregular acinar and ductular structures or tubulopapillary pattern surrounding large areas of cystic cavitation which contained abundant pale eosinophilic to amphophilic secretion effacing normal architecture. The cells had round ovoid hyperchromatic nuclei with finely stippled chromatin and occasional centrally located nucleoli. The cytoplasm is scant to moderate eosinophilic with indistinct cell borders. Many acini contained pale eosinophilic homogeneous secretion. There was marked hydronephrosis with compression atrophy of the medulla.
Microscopic Findings: Renal Papillary Tubular Cystadenocarcinoma with Hydronephrosis
Comments:
Renal adenocarcinomas are rapid growing tumors and more prone to metastasis. Metastasis usually has occurred by the time the tumor is diagnosed. In dogs, 50-70% of renal cell carcinomas metastasize. The most likely sites are lung, liver and regional lymph node. The survival ranges for carcinomas was 0-59 months (median 16 months). Renal adenocarcinomas have propensity for invasion of the renal vein and may ascend up the posterior vena cava with early and frequent formation of pulmonary metastasis. Metastasis may also be seen in the liver, adrenals, and vertebrae. Widespead metastasis is common.
Special Thanks to St. Charles Animal Hospital and Antech for the interesting case and follow-up.
August's Case of the Month- 2022
Sonographer: Emily Evans, BVM&S
Visceral Mast Cell Tumor
PATIENT INFORMATION:
Age: 11yo
Gender: Female Spayed
Species: Canine
Breed: Golden Retriever
Weight: 63lbs
HISTORY:
Previously healthy. Initially presented for vomiting and diarrhea with a normal appetite. Treated for clostridium and spirochetes with supportive care, probiotics and metronidazole. Barium study performed with no evidence of obstruction or foreign material was also performed. Presented the next day to the emergency clinic for persistent vomiting and diarrhea. Repeat radiographs show reduced cranial abdominal detail and hepatomegaly. No free fluid noted on AFAST. Represented to primary veterinarian one week later with blood in stool, febrile with mild neutrophilia and monocytosis. No reported history of mass removals, FNAs or biopsies.
ULTRASOUND FINDINGS:
Liver - Moderate-severely increased size, rounded shape and moderately coarse hyperechoic echogenicity with an ill-defined hypoechoic small mass in the left liver. (3.1x2.7cm)
Spleen- The spleen was moderately enlarged(3.1cm), elongated, and rounded in shape with a coarse echotexture. There was a cavitated capsule altering small mass in the tail of the spleen(2.3x2.1cm)
Lymph nodes - Multiple mesenteric lymph nodes were moderate-severely enlarged with rounded shape having a mottled mildly hypoechoic echogenicity.(at least 7.6cm in length and 2.9cm in depth) The medial iliac lymph nodes were mildly plump with an isoechoic echogenicity. Lt/Rt: 0.8/0.7cm
Gastrointestinal Tract - The stomach had increased wall thickness with some areas of hypoechoic hazy loss of layering detail.(6.5-7.3mm) The pylorus was free of obstruction. Many loops of the small intestine had increased wall thickness with disproportionately large mucosal layers. Some loops had hazy hypoechoic loss of layering detail. There was echogenic stippling throughout the mucosal layers. The bowel had mildly increased overall motility with liquid contents. The colon had normal to mildly increased wall thickness and normal layering. No focal intestinal masses or obstructions identified. Duodenum 5.6-6.0mm, Jejunum 3.7-5.9mm, Colon 3.0mm
Mild ascites noted throughout the abdomen.
SELECT IMAGES:
Image 1: Splenomegaly and cavitated splenic lesion.
Image 2: Gastric wall thickening with hazy layering detail loss
Image 3: Severely enlarged and hypoechoic mesenteric lymph node.
Diagnostic tests performed:
Ultrasound guided fine needle biopsies of the spleen and mesenteric lymph nodes were collected.
Diagnosis
Spleen: Mast cell tumor
Mesenteric lymph node: Mast cell tumor
Cytology Comments
The diagnosis of a mast cell tumor is definitive (100% confidence), for both locations, consistent with a metastatic process. The slides from the two locations appear fairly similar, are moderately to highly cellular and consist of few to many red blood cells and a nucleated cell population predominated by mast cells with few small lymphocytes and rare plasma cells. The mast cells have a moderately to well granulated cytoplasm that surrounds a centrally located round nucleus with loosely clumped chromatin pattern. Anisokaryosis and anisocytosis are mild to moderate. Many purple granules are present in the background.
Cytology Images:
Image 4: Lymph Node aspirate - Several mast cells with fewer small lymphocytes and a plasma cell*Image provided by Eastern VetPath
Image 5: Speen- Numerous mast cells*Image provided by Eastern VetPath
CASE OUTCOME:
Patient was started on steroids however her clinical signs progressed and due to her grave prognosis she was humanely euthanized the following day.
PROGNOSIS/DISCUSSION:
The diagnosis of primary visceral mastocytosis is uncommon in canine patients. The liver, spleen and gastrointestinal tract are the most common sites for primary visceral MCT. It is possible that the splenic mass in this case was the primary tumor. The prognosis in these cases is poor and diagnosis is often delayed due to non-specific clinical signs(Vomiting/Diarrhea/Anorexia)
References:
Garrett L. Canine mast cell tumors: diagnosis, treatment, and prognosis. Vet Med (Auckl). 2014;5:49-58
https://doi.org/10.2147/VMRR.S41005
Takahashi T, Kadosawa T, Nagase M, Matsunaga S, Mochizuki M, Nishimura R, Sasaki N. Visceral mast cell tumors in dogs: 10 cases (1982-1997). J Am Vet Med Assoc. 2000 Jan 15;216(2):222-6. doi: 10.2460/javma.2000.216.222. PMID: 10649758
Special thanks to Dr. Emily Fant at Shady Grove Animal Clinic and Dr. Casey Leblanc at Eastern VetPath.